Achieving Racial Equity in Oral Health Among Distressed Populations Amid COVID-19
Terrell Strayhorn*
Department of Evelyn Reid Syphax School of Education, Virginia Union University, USA
*Corresponding author: Terrell Strayhorn, Department of Evelyn Reid Syphax School of Education, Virginia Union University, USA
Article History
Received: March 01, 2021 Accepted: March 05, 2021 Published: March 10, 2021
Citation: Strayhorn T. Achieving Racial Equity in Oral Health Among Distressed Populations Amid COVID-19. Int. Jr. Infect Dis & Epidemlgy. 2021;2(1):09‒10. DOI: 10.51626/ijide.2021.02.00003
Abstract
This short communication frames an overview of racial equity gaps in oral health and describes how COVID-19 prevalence among distressed populations exacerbates disproportionate impacts that existed prior to the pandemic. Racialized oral health gaps compounded by COVID-19 affects their general and public health. Implications for policy and practice are highlighted.
Keywords: Oral healthcare; Racial equity; Dental services; Minority; Social determinants of health
Short Communication
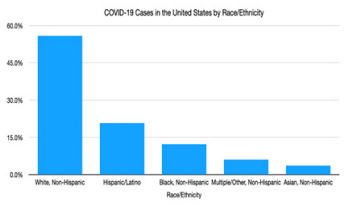
Achieving racial equity in oral health is a major goal of global policy that drives national health campaigns and more local public health agencies. Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2), hereafter COVID-19, prevalence complicates efforts to systematically address racial health disparities. Recent data continue to show that COVID-19 disproportionately impacts people of color. According to Johns Hopkins University (most recent data at time of writing), there were 109 million COVID-19 cases in the world, 27.6 million cases in the United States, and nearly 45% of US cases were among Black, Indigenous, People Of Color (BIPOC) although these groups together represent just over one-third of the US population (Figure 1). Pre-existing oral health inequities experienced by Underrepresented Minorities (URMs), such as dental caries and oral cancer, have been magnified by COVID-19 [1,2]. For instance, we observed large racial/ethnic gaps in tooth loss among URMs (25%) compared to 10% for Whites prior to the pandemic [3,4].
Figure 1: COVID-19 Cases in the United States by Race/Ethnicity.
Not only have we seen COVID-19 have a higher disproportionate impact on BIPOC, but it has greater concentration in communities of color and leads to a significantly higher death rate among Black1 Americans. Nationally, Black Americans account for 15.7% of all COVID-related deaths (of known race), but only represent 12.4% of the country’s population. COVID-related racial inequities persist at the state level. For instance, in Michigan, Blacks make up 17% of the total state population but comprise 40% of COVID-related deaths. In New York, Blacks make up 14% of the state’s population but 23% of COVID-related deaths. And, startlingly, Blacks are 75% of COVID-related deaths in the District of Columbia (DC), although they represent just 45% of the district’s population. Close monitoring (or surveillance) of where and to what extent COVID-19 mortality is inequitably impacting BIPOC communities is critical for guiding the success of public and/or oral health policy and programmatic responses.
There are myriad root causes for the inequitable impact of COVID-19 on the oral and physical health of BIPOC communities in the United States. For instance, a long line of research has shown that conditions in the places where people live, learn, work, and leisure affect a wide range of health outcomes [3,4], including oral health [5]. These social determinants of health include limited access to quality education, few healthcare providers (especially professionals of color) or hospitals, poor health insurance, and greater exposure to health risks related to job or occupational hazards [5,6]. For example, 34% of frontline or essential workers in the US are Black or Latinx, though they constitute less than one-third of all US workers. Nearly 40 million frontline workers work in close physical proximity to others, tend to be less educated than the wider workforce and earn below-average wages that offer little to no health insurance [7], such as dental coverage. These points are important to note so as to avoid blaming the individual as the creator of their own crisis; rather, critical analyses, of this kind, point to structural and systemic drivers of racial inequities and reveal how structural factors-like citizenship, (dis)ability, poverty—influence aspects of BIPOC individual and community health before, during, and after COVID-19.
It is clear that as COVID-19 cases and related deaths continue to grow by record-setting increases each day, so too do the emotional and psychological tolls on vulnerable populations and distressed communities. With Blacks and Hispanics dying from COVID-19 at rates higher than their proportion in the population, they are more likely to know someone who has died of the disease. One Washington Post poll estimated 1 in 3 Black Americans know someone first-hand who has died by the virus, far exceeding White counterparts [8]. Consequently, another report indicated elevated grief and psychiatric problems among socially disadvantaged groups [9]. A wealth of emerging evidence further suggests the need to examine the short- and long-term effects of racial trauma on BIPOC pandemic survivors; racial trauma refers to real or perceived discrimination that damages physical and mental health through chronic, repeated exposure to stress [10]. For instance, Asian communities have experienced an uptick in discrimination because of the coronavirus outbreak originating from China according to most reports [11]. As if this is not enough, populations vulnerable to COVID-19 infection, mortality, and pandemic-related psychological impacts are also at higher risk for oral health problems and periodontal diseases [12,13]. COVID-19 only further exacerbates the situation by restricting access to care due to state-mandated “stay at home” orders in some areas, clinic closures, reduced hours, and limited non-urgent dental visits [14].
But there’s hope on the horizon. As therapeutics and vaccines for COVID-19 gain Federal Drug Administration (FDA) emergency approval and governments launch massive testing and vaccination sites, preliminary data suggest a “flattening of the curve” and some modest reduction in cases among socioeconomically distressed communities. Public health advisories to wear face coverings, practice daily hygiene, and physically distance also help curb the spread of infection. Greater compliance with public health guidelines allows some states to relax strict “stay-at-home” orders, which permit some providers to open up dental clinics, expand operating hours, and accommodate routine care visits. Rapid technological advances, free virtual conferencing applications (e.g., Skype, Zoom), and social media help us all stay connected, even while physically six feet apart. Though no replacement for in-person human connections, online, virtual, computer-mediated communication and contact can foster community and sense of belonging, which is a basic human need [15].
aThroughout this article, I use the terms “Black” and “African American” interchangeably to refer to people of African descent (e.g., West Indian, Haitian, African) living in the US.
bBy “frontline worker,” I refer to those brave, valiant members of the workforce who must physically report to their job sites and risk their personal health in the face of unknown threats to ensure the collective well-being, continuity, and safety of the economy, businesses, and each of us, in keeping with Department of Homeland Security (DHS) regulations. They might include bus drivers, grocery workers, butchers, barbers, delivery service drivers, correctional officers, and public health/healthcare providers, especially oral health specialists.
References
- Northridge M, Kumar A, Kaur R (2020) Disparities in Access to Oral Health Care. Annual Review of Public Health 41(1): 513-535.
- Clancy C (2003) Health Services Research: From Galvanizing Attention to Creating Action. Health Serv Res 38(3): 777-782.
- Gilbert G, Paul Duncan R, Shelton B (2003) Social Determinants of Tooth Loss. Health Serv Res 38(6p2): 1843-1862.
- Finlayson T, Williams D, Siefert K, Jackson J, Nowjack Raymer R (2010) Oral Health Disparities and Psychosocial Correlates of Self-Rated Oral Health in the National Survey of American Life. Am J Public Health 100(S1): S246-S255.
- Sabbah W, Tsakos G, Sheiham A, Watt R (2009) The effects of income and education on ethnic differences in oral health: a study in US adults. J Epidemiol Community Health 63(7): 516-520.
- Chavers L, Gilbert G, Shelton B (2002) Racial and Socioeconomic Disparities in Oral Disadvantage, a Measure of Oral Health-related Quality of Life: 24-month Incidence. J Public Health Dent 62(3): 140-147.
- Tomer A, Kane J (2020) To protect frontline workers during and after COVID-19, we must define who they are. Brookings Metro COVID-19 Series.
- Goldstein A, Guskin E (2020) Almost one-third of Black Americans know someone who died of COVID-19, survey shows. The Washington Post.
- Purtle J (2020) COVID-19 and mental health equity in the United States. Soc Psychiatry Psychiatr Epidemiol 55(8): 969-971.
- Comas Diaz L, Hall G, Neville H (2019) Racial trauma: Theory, research, and healing: Introduction to the special issue. American Psychologist 74(1): 1-5.
- Travernise S, Oppel R (2020) Spit on, yelled at, attacked: Chinese-Americans fear for their safety. The New York Times.
- Barrow S, Xionan X, Le Geros A, Mijares D, Le Geros R, et al. (2003) Dental caries prevalence among a sample of African American adults in New York City. Dent Clin North Am 47(1): 57-65.
- Kisely S (2016) No Mental Health without Oral Health. Can J Psychiatry 61(5): 277-282.
- Coke C, Davison B, Fields N, Fletcher J, Rollings J, et al. (2021) SARS-CoV-2 Infection and Oral Health: Therapeutic Opportunities and Challenges. J Clin Med 10(1): 156.
- Strayhorn T (2019) College students’ sense of belonging: A key to educational success.