Neuropsychiatric Approaches for Human Suicide Prediction and Management
Da-Yong Lu*, Hong-Ying Wu
School of Life Sciences, Shanghai University, China
*Corresponding author: Da-Yong Lu, School of Life Sciences, Shanghai University, Shanghai200444, PRC, China
Article History
Received: October 09, 2021 Accepted: November 09, 2021 Published: November 12, 2021
Citation: Da-Yong Lu, Hong-Ying Wu. Neuropsychiatric Approaches for Human Suicide Prediction and Management. Int J Neuropsy Beh Sci. 2021;2(3):87‒91. DOI: 10.51626/ijnbs.2021.02.00019
Abstract
Human suicide accounts for 2% Human mortality worldwide. Some widely accepted medical knowledge suggests that suicide events or episodes are strongly associated with neuropsychiatric events and changes. We previously accumulate data and evidence that neuropsychiatric study and interference may help us to reduce suicide rates and mortality. Given the useful evidence and therapy in the clinic, cutting off unnecessary suicide-induced genes or molecules will ultimately reduce suicide-induced mortality in statistically significant manner. This article discusses how the genetic, epigenetic and molecular phenotypes can be manipulated in the lab animals and a framework of neuropsychiatric changes and interferences in patients. Possible drug targets and treatments are also discussed.
Introduction
General and historic information
Human suicide accounts for 2% Human mortality worldwide [1]. A great number of risk factors may trigger human suicide ideation and episode [2-4]. It had a long history for human suicide reports [5,6] (Table 1). However, it is still a complex and mystery issue for how risk factorials promote suicide ideation and behaviors. Among these different risk factors, neuropsychiatric changes are indispensable.
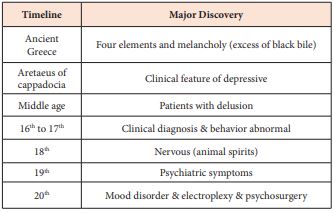
Table 1: Historic order of knowledge discovery for mood disorder (suicide associated).
After a length period of psychiatric onset and pathophysiology turmoil, “patients” may seek suicide action to end their painful emotion and depressive syndromes. Through this lengthy duration of psychiatric abnormality, the functional change in “patient brain” may drive insane condition (end of life unconsciously) [5-8]. This medical hypothesis can answer why fatal phenotype (human suicide) emerge after a sequential and cascade of pathological pathways and networks [4].
Past evidence in the clinic
Medical evidence suggested that suicide events or episodes are associated with wide variables (inside and outside) [9]. Mental condition diagnosis and prevention may come from it [10-12]. In order to find useful measures, mental-related genes or molecules should be identified first. Only by this pathway, suicide prediction and prevention can be possible.
Neuropsychiatric Field
Neuropsychiatric behaviors and knowledge
It is easy to note that outside force may lead to human suicide. But, we disparately need to know why some one chose suicide while most others stay calm. This personal variation may be identified by clinical clue and association of interpersonal variation of biochemistry and neuropsychiatry. Whether therapeutic responses can reduce patient’s situation [8-12]? Neuropsychiatric approaches may provide such biomedical insights. Identical signs of depressive or manic, brain images, biochemical parameters and instrumental data should be carefully associated. As a result, several dimensions of “mental diseases” have been estimated.
Biological basis
Until now, scientists do not well confirmed for suicide origins (framework of psychiatric syndrome and neuropathy in image data and biochemical assays) by existing techniques. Human suicide events and mental illness dimensions are comparable for biochemical parameters and environmental variables. Different evaluative systems should be given for suicide diagnostics and therapeutic selection (Table 1). Biomedical diagnostic paradigms and novelty should be pursued in the future.
Human suicides were previously managed by chemical drugs, mainly antidepressants and other anti-psychiatric agents. However, these drug therapies like a double-edged sword that has both strengths and weaknesses [13-22]. Only part of depressive patients is effective with chemical drugs. Some of depressive patients even commit suicide. To many depressive persons, current antidepressants and drug selective systems are useless [13]. In order to achieve higher therapeutic responses, therapeutic mechanisms and new medication should be explored.
Clinical prediction and diagnosis
Before high-quality therapeutic drug development, biomedical diagnostic paradigms should be established. Previously, suicide/mental illness diagnostics came from patient’s psychiatric symptom and behaviors [7,8]. These psychiatric symptoms can only be diagnosed by well-trained psychiatrists. These symptoms (psychoanalysis) have been classified. Mental health diagnosis and confirmation based on patient’s symptom checklist, genetic analysis and signal circuits should all be studied. Transition of symptom diagnosis into biomedical parameter prediction is indispensable [4,5].
Genetic and molecular studies
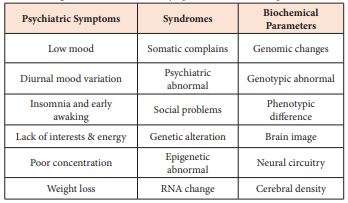
Detail diagnostic information (Diagnostic and Statistical Manual of Mental Disorder—from DSM-I to DSM-V of mental problems and Hamilton Depression Rating Scale (HAM-D) of suicide risks) will be further progressed. New approaches will been seen from Table 2.
Table 2: Diagnostic translation from symptoms to biochemical parameters.
To find and identify interaction and association between psychiatric symptoms, biological parameters (genetic or molecular variation), synaptic activity (hormone or transmitter levels) and neuropathy (structure and function) play key roles of neurobiology in patients between high suicide risks and normal people in Table 2. By doing this etiologic/pathologic evaluation, clinical evidence can be gradually transformed.
Psychopathologt
Mental disorders verses suicide
Pathogenesis for suicide behaviors may come from genomic alteration induced by consistent outside irritations. From psychiatric scope, the depressive or mania symptoms are divided. Genetic elements and variations (inheritable, mutation, relocation, copy number and epigenetic) may be characterized from features of suicide risks, events or drug toxicity using these aspects of information. Human neuropathy evidence may profoundly impact for human suicide study [10-12].
To evaluate human suicide in neuropathy (nature, pathways and network), new neurobiology knowledge (structure, function and chemistry) for mental disorders and suicide should be accumulated and compared [20-22]. The mystery and complex processes of neuropathology have been evidenced in brain image and molecular analysis in the past reports [23-32]. Different patterns of neural structural and functional elements were carried out in the past. This neuropathy characterized as brain lesion, density, structure and image may be as informative.
Diagnosis-therapeutic relation
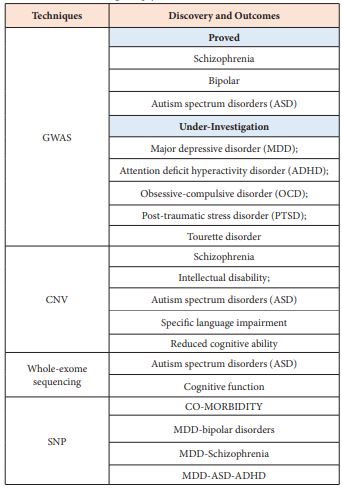
Knowledge breakthrough of suicide prediction and therapy is supported by different technology. Like many other biomedical disciplines, hospital equipment and technical supports play key roles for suicide prediction and therapeutic decision-making in the clinic. Previously, an association between the severity of drug side-effects (suicidal incidence in juvenile) and drug responses (patients’ depressive symptom alleviations) [13-21] had drawn unprecedented attention for repeated suicide episodes, self-harm or self-injures. Comparison of similarity and diversity of diagnosis, drug toxicity, metabolism and responses should be boosted (Table 3). By upholding these efforts, advanced suicide predictive and treatment systems might be achieves in general hospitals.
Table 3: Genetic knowledge for psychiatric diseases.
Possible molecular-based diagnosis of depression or suicide will gradually enter into the hospitals. Many environmental factors could be ruled out in therapeutic decision-making. Cerebral morphological change and pharmacogenomics (PG) provided with new biomedical foundation [24-29]. To stratify pathology and clinical data from plethora environmental variables, more biomedical diagnosis should be boosted. Calculation of GWAS (genome wide association study) provides wealth of information [30,31]. Genomic information between normal and genetic vulnerable humans has to be scaled up globally more recently [9-12]. Only human genetic data of neural dysfunction and family diseases in larger sample sizes (>100,000 human subjects) can discover new psychiatric knowledge and diagnostic paradigms.
Neurosciences
Brain anatomy and circuitry
Different psychiatric symptoms, synaptic connectivity, neural circuitry and brain function continue to decipher; different cerebral locations, entities and domains are vulnerable to dysfunctional architecture of mental cognitive, emotion and behaviors; Regional lesion or destruct of brain circuitry may lead to abnormal psychiatric symptoms, diseases and human suicide. They are represented into two neural-chemical systems; Dopamine associated areas: ventral striatum (VS), amygdale, orbitofrontal cortex (OfC) and anterior cingulated (ACC); Serotonin associated areas; amygdala, lateral OfC, insula and hypothalamus;
[32].
Neurobiology
Brain genotypic and phenotypic alteration associates with different dimensions of mental disorders [33-35]. This clinical evidence of different psychiatric symptoms (mood disorders; opposite extremes of emotional symptoms and biomedical profiles—anxiety and depression), schizophrenia (high-level of dopamine) and neurodegenerative disorder (low level of dopamine; cognitive impair, such as Alzheimer and Parkinson’s diseases) began to accumulation. It is very useful for suicide diagnosis and treatment in the clinic.
Modern diagnosis
Since human suicide might be a brain disease, brain image changes of both cerebral volume and regional lesion (prefrontal or cingulated cortex and so on) are useful ways, such as position emission tomography (PET), single-photon emission computed tomography (SPECT), electroencephalogram or functional magnetic resonance imaging (fMRI) [24-29]. The changes in cortical and sub-cortical areas may be especially relevant for suicide diagnosis in the future.
Divergent techniques of neural imaging are taken together to identify cerebrally morphological changes in brains and guide proper therapeutic selections consequently. To overcome false-positive or false-negative diagnostics, software or artificial intelligence techniques are useful for suicide diagnosis in morphological evaluation.
Neural transmitters
Signal pathways (activators and inhibitors) in neurobiology are modulated by neural transmitter, its receptors, signal cascade processes, breakup-enzymes and signal transduction. This field of neurotransmitter knowledge is more straightforward than those of psychoanalysis and other observation.
Dopamine network is associated with human reward machinery (cognitive); Decreasing of dopamine levels may lead to neurodegenerative diseases and increasing dopamine production may lead to schizophrenia symptoms, pathological gambling and hypersexual activity [32].
Serotonin network and pathway is associated with emotional activity and symptoms (anxiety—aversion); some emotional changes are greatly correlated with human suicide and mortality [32].
Normal human brains are soft and low density from outside observations. However, some aberrantly poly-materials, such as Tau and β-amyloid are commonly observed in patients with neural-degenerating diseases (Alzheimer and Parkinson’s diseases). In these neurodegenerative diseases, molecular dysfunctions are really matters that are straightforward for brain image and circuitry observation.
Therapeutic Management
Drug responses and targets
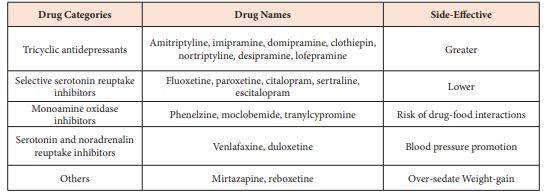
Drug development for human suicide was coming from anti-psychiatric drugs now [7-8, 33,34] (Table 4). Detailed information and targets will be carried out further. These therapeutic targets and selection should be based on molecular or morphological diagnosis.
Table 4: Different types of antidepressants and pharmacological characteristics.
Discussion
Association between psychiatry and suicide
The earliest reports for human suicide did not use the term of “suicide”’. It commonly describes clinically symptoms—melancholy (current language as depression) or other clinical term “mania”. It is not until 17th century (AC 1642) that word “suicide” was formally named [3]. The genetic or molecular-based association between psychiatry and suicide will be revealed in the future.
Two extremes of psychiatric symptoms (depression and mania) are deeply rooted in suicide ideation and behavior. It needs advanced knowledge to categorize and integrate suicide and psychiatry in deeper neurobiology challenge and insights.
Knowledge novelty
The relationship between risk-factorials of chemical, genetic, molecular, cellular, environmental, social and therapeutic targets should be integrated in the future. The knowledge gaps between suicide and psychiatry should be filled in the near future. We look forward to a great integration of these different factorials and treatment of different symptoms with similar drugs (kill several birds by one stone).
Presently, many unresolved questions of why no unequivocally evidence that can reveal variations between normal and suicide-risk humans. Environmental forces or genetic variation can be integrated into modern diagnostic parameters and therapeutic targets. A scale-up comparison between suicide and mental health problems by modern technology will be further carried out. Some unexpected scientific discovery and achievement may bring us into new horizons. As a result of all, neuropsychiatric efforts cannot be overlooked.
Future Direction
Major breakthroughs
• Suicide risk prediction and diagnosis should be more straightforward (molecular-or morphological-based).
• Neuropsychiatric knowledge about signal pathways, such as neural transmitter receptors, signal cascade and neurotransmitter activators/inhibitors should be especially emphasized because some well-known psychiatric paradigms are based on that.
• Mathematical, algorithmic, computational network and artificial intelligence for suicide should be emphasized (equation, modality and large databases of genetic, bioinformatics or brain image data available).
• New animal models, state-of-the-art techniques and avant-garde lab instruments, such as gene knockout, optogenetics, genomic editing or genetic engineering mice should be used in drug developments, licensing and clinical utilities.
• Seeking genetic or bioinformatics variations from genomic data beyond protein-encoding sequencing regions (many repeat DNA in human genomes).
• New series of drug targets, mechanisms and development strategies [35-45].
Genetics-environmental interplay
Accumulate advanced knowledge about suicide etiologic and pathologic association needs multi-disciplinary neuropsychiatry study. Modern diagnosis should be based a sequence from genetic to bioinformatics to visual data or vice versa. Presently, we do not know which pathway is quicker and more effective. Yet, further medical exploration on suicide neurobiology should be greatly fruitful.
Conclusion
In summary, the clinical suicidal behaviors and events should not be confined in suicide episode and behaviors. Chemical structures of drugs, genetic backgrounds of patients and environmental variables should be overall carried out. More cutting-edge technology, high-quality statistical analysis and artificial intelligence for larger number of patients should be integrated by different systems of modern diagnostics.
References
- Bondy B, Buettner A, Zill P (2006) Genetics of suicide. Mol Psychiatry 11(4): 336-351.
- Kapur N, Gask L (2009) Introduction to suicide and self-harm. Psychiatry 8(7): 233-236.
- Shandilya S (2018) Suicide and suicide prevention: a historical review. The Research Journal of Social Science 9(12): 35-40.
- Lu DY. Suicide Risks and Treatments, New Ideas and Future Perspectives. In: Da-Yong Lu (eds.), Nova Science Publishers: USA; 2017.
- Lu DY, Wu HY, Cao S, Che JY (2020) Historical analysis of suicide. J Translational Genetics & Genomics 4: 33.
- Marneros A (2009) Mood disorders: epidemiology and natural history. Psychiatry 8(2): 52-55.
- McAllister-Williams R, Ferrier IN (2009) Pharmacological management of bipolar affective disorder. Psychiatry 8(4): 120-124.
- McAllister-Williams R, Ferrier IN (2009) Pharmacological management of unipolar affective disorder. Psychiatry 8(4): 113-119.
- Lu DY, Lu TR, Zhu PP, Che JY (2016) The efficacies and toxicities of antidepressant drugs in clinics, building the relationship between Chemo-Genetics and Socio-Environments. Cent Nerv Syst Agents Med Chem 16(1): 12-18.
- Malhotra D, Sebat J (2012) CNVs: harbingers of a rare variant revolution in psychiatric genetics. Cell 148: 1223-1241.
- Krystal JH, State MW (2014) Psychiatric disorders: diagnosis to therapy. Cell 157(1): 201-214.
- Lu DY, Che JY, Wu HY, Lu TR, Putta S (2020) Suicide risks and prevention, neuropathogenic study. Psychiatry 4(1): 124.
- Lu DY, Wu HY, Xu B (2021) Pathology study for human suicide. Health and Primary Care 5: 1-4.
- Marshall M (2020) Roots of mental illness. Nature 581: 19-21.
- Brent D, Melhem N, Turecki G (2010) Pharmacogenomics of suicidal events. Pharmacogenomics 11(6): 793-807.
- Lu DY, Lu TR, Zhu PP (2012) How can we pinpoint genetic involvement in antidepressant-induced suicide? Adv Pharmacoepidemiol Drug Safety 1(1): e101.
- Lu DY, Lu TR, Zhu PP (2012) Genetics in neural toxicities of drugs. Central Nervous System Agent Medicinal Chemistry 12(4): 250-253.
- Lu DY, Lu TR, Zhu PP (2013) Pharmacogenetics in neural toxicities of drugs. Pharmacogenomics 14(10): 1129-1131.
- Lu DY, Lu TR, Che JY, Zhu PP (2014) Genetics and bioinformatics studies of antidepressant drug therapeutic efficacies and toxicities, a current overview. Recent Pat CNS Drug Discov 9(3): 193-199.
- Lu DY, Lu TR, Zhu PP (2010) Undesired neural side-effects of a drug, a chemical and genetic interrelated problem. Central Nervous System Agents in Medicinal Chemistry 10(2): 108-112.
- Zhao Y, Xiong N, Liu Y, Zhou YH, Li NM, et al. (2013) Human dopamine transporter gene: differential regulation of 18-kb haplotypes. Pharmacogenomics 14(12): 1481-1494.
- Youngtrom IA, Strowbridge BW (2012) Visual landmarks facilitate rodent, spatial navigation in virtual reality environment. Learn Mem 9(3): 84-90.
- Read J, Runciman O, Dillon J (2016) In search of an evidence-based role for psychiatry. FSOA 2(1): FSO101.
- Frangou S (2009) Brain structural changes in mood disorders. Psychiatry 8(3): 105-106.
- Roiser JP, Rubinsztein JS, Sahakian BJ (2009) Neuropsychology of affective disorders. Frangou S. Brain structural changes in mood disorders. Psychiatry 8(3): 91-96.
- Desmyter S, Bijttelier S, Heeringen KV (2013) The role of neuroimaging in our understanding of the suicidal brain. CNS & Neurological disorders Drug Targets 12(7): 921-929.
- Frangou S (2008) Functional neuroimaging in mood disorder. Psychiatry 6(3): 102-104.
- Jiang JJ, Yan ZZ, Sheng C, Wang M, Guan QL, et al. (2019) A novel detection tool for mild cognitive impairment patients based on eye movement and electroencephalogram. J Alzheimer’s disease 72: 389-399.
- Miller G (2016) Brain scans, a prone to false positive study says. Science 353(6296): 209.
- Menke A, Samann P, Kloiber S, Czamara D, Lucae S, et al. et al. (2012) Polymorphisms within the metabotropic glutamate receptor 1 gene are associated with depression phenotypes. Psychneuroendocrinology 37(4): 565-575.
- Menke A, Domschke K, Czamara D, Klengel T, Hennings J, et al. (2012) Genome-wide association study of antidepressant treatment-emergent suicidal ideation. Neuropsychopharmacology 37(3): 797-807.
- Ramsay TZ, Skov M (2010) How genes make up your mind: Individual biological differences and value-based decisions. J Economic Psychology 31: 818-831.
- Lu DY, Wu HY, Cao S, Che JY (2021) An overview of suicide study. EC Psychology & Psychiatry 10(3): 37-43.
- Lu DY, Lu TR (2021) Drug discovery for suicide management. EC Pharmacology & Toxicology 9(11): 76-86.
- Lu DY, Zhu PP, Wu HY, Yarla NS, Zhu H, et al. (2016) Human suicide study, is there an associations between suicide and mental illness? Metabolomics 6(3): 186.
- Lu DY, Zhu PP, Wu HY, Yarla NS, Xu B, et al. (2018) Human suicide risk and treatment study. Cent Nerv Syst Agents Med Chem 18(3): 206-212.
- Na EJ, Lee H, Myung W, Fava M, Mischowlon D, et al. (2019) Risks of completed suicide of community individuals with ICD-10 disorders across age groups: A nationwide population-based nested case-control study in South Korea. Psychiatry Investig 16(4): 314-324.
- Pennisi E (2010) Shining a light on the genome’s ‘dark matter’. Science 330(6011): 1614.0
- Freedman DH (2019) Hunting for new drugs with AI. Nature 576: s49-s53.
- Walhekar V, Birajdar P, Bagul C, Kumar D, Muthal A, et al. (2021) Artificial intelligence: Drug discovery and development prospective in medicinal chemistry. EC Pharmacology & Toxicology 9(11): 87-92.
- Lu DY, Shen Y, Cao S (2020) High quality treatments for human suicidal events and mortality. Advanced Techniques in Biology & Medicine 8(2): 269.
- Vanneste S, Ridder DD (2021) Chronic pain as a brain imbalance between pain input and pain suppression. Brain Communication 3(1).
- Mann JJ, Michel CA, Auerbach RP (2020) Improving suicide prevention through evidence-based strategies: A systematic review. Am J Psychiatry 178(7): 611-624.
- Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, et al. (2020) Understanding the complex of suicide in depression: from research to clinics. Psychiatry Investig 17(3): 207-221.
- Lu DY, Wu HY, Lu TR (2020) Human suicide study, new insights and drug development. Indian J Community Medicine 3(1): 1028.