Role of Experience in Developing an Interventional Nephrology Program at an Academic Center in Pakistan
Ali Raza Khan1*, Anila Jasmine1, Fawad Qureshi2
1Department of Medicine, Aga Khan University Hospital, Pakistan
2Division of Nephrology and Hypertension, Mayo Clinic Rochester, USA
*Corresponding author: Ali Raza Khan, MD, FASN, FASDIN, Aga Khan University Hospital (AKUH), Stadium Road, P.O. Box 3500, Karachi 74800, Pakistan
Article History
Received: July 26, 2021 Accepted: August 20, 2021 Published: August 24, 2021
Citation: Khan AR, Jasmine A, Qureshi F. Role of Experience in Developing an Interventional Nephrology Program at an Academic Center in Pakistan. Int J. Hert & Vasclr Syst. 2021;2(1):16‒21. DOI: 10.51626/ijhvs.2021.01.00004
Abstract
Background: A well-functioning vascular access is the backbone of renal replacement therapy in chronic kidney disease (CKD). Vascular access management is largely done by vascular surgeons and interventional radiologists who are often unaware of its impact and repercussions in the care of dialysis patients. This has led to delayed dialysis, temporary vascular access, hospitalization, and other associated morbidities. Interventional nephrology is a subspecialty of nephrology that increases the involvement of nephrologists in vascular access procedures. The advent of interventional nephrology as a field has not only improved continuity of care but has also led to uninterrupted dialysis treatments and decreased rate of hospitalization.
Methods: We established a new interventional nephrology service at the Aga Khan University Hospital, Karachi, Pakistan with the help of an interventional nephrologist accredited by the American Society of Diagnostic and interventional nephrology (ASDIN). The study aims to an arrangement of equipment, and training of staff to assist in procedures.
Results: To date, we have placed 20 tunneled dialysis catheters (TDCs), performed 8 arteriovenous fistula (AVF) venoplasty procedures, some venous mapping procedures as well as renal biopsies all in an outpatient setting with good outcomes. We further plan on starting a peritoneal dialysis catheter placement program at our center soon.
Conclusion: In a country like Pakistan where resources are limited, interventional nephrology can provide good vascular access care and timely interventions for vascular access dysfunction while allowing the procedures to take place in an outpatient setting, hence minimizing costs. The current study program may be a guide to help establish a similar program by other specialties with the support of the hospital administration.
Keywords: Interventional nephrology; Vascular access; Chronic kidney disease; End-stage renal disease; Dialysis
Introduction
Chronic Kidney Disease (CKD) contributes to significant morbidity and mortality from non-communicable diseases. In 2017, the prevalence of CKD in Pakistan was reported to be more than 14 million, with nearly 37000 attributable deaths [1]. In Pakistan, the incidence of end‐stage renal disease (ESRD) is estimated to be about 100 patients/million population [2]. As the country’s population crosses 250 million, it is no surprise that patients on dialysis therapy are increasing dramatically [3].
Pakistan is a resource-limited country that lacks a coordinated and comprehensive health system. In 2017, only 2.90% of the GDP was allocated to healthcare [4]. As a Lower-Middle-Income Country (LMIC), most of the focus of health initiatives has been on communicable diseases. Meanwhile, non-communicable diseases like CKD, which are becoming a major health burden with increasing urbanization, have not received much attention [5,6].
Management of patients in nephrology has historically relied on procedures. For this reason, nephrologists have designed and developed instruments to evaluate and manage kidney disease. These include the biopsy gun for kidney biopsy, the hemodialysis shunt, double-lumen tunneled dialysis catheters (TDC), arteriovenous fistulas (AVF) and arteriovenous grafts (AVG) for hemodialysis, tunneled catheter, and laparoscopic peritoneal dialysis catheters (PDC) [7]. In fact, a nephrologist, Dr. J Holmes is considered the father of diagnostic ultrasound; a modality that is used across all specialties of medicine [8].
However, over time vascular access management was taken up by other specialties like vascular surgery and interventional radiology, which in most cases were not aware of the impact and repercussions in the care of dialysis patients. This transfer has been attributed to a shortage of nephrologists, heavy patient burden, a lack of emphasis on procedures during training years as well as decreased interest by nephrologists because other areas of nephrology seemed scientifically more rewarding [9,10].
Although dialysis has revolutionized the management of patients with ESRD, the need for vascular access has contributed to the associated morbidity and mortality and is the leading cause of hospitalization in this patient population [11]. Typically, dialysis access procedures have been given low priority by surgeons and radiologists who perform these procedures which results in delays in the initiation of therapy [3]. As a result, patients require frequent hospitalization and placement of TDCs at the bedside.
Interventional nephrology is a dynamic subspecialty of nephrology that gives control of dialysis access management back to where it belongs. It deals with ultrasonography of kidneys and ultrasound-guided biopsy for diagnostic purposes, insertion of PDCs for peritoneal dialysis, insertion of TDCs as vascular access for patients undergoing hemodialysis, and percutaneous endovascular procedures to manage dysfunctional AVFs/AVGs in ESRD patients. The advent of interventional nephrology has led to a marked decrease in dialysis patient hospitalization and uninterrupted dialysis treatments [12]. Therefore, nephrologists have taken the initiative to perform these procedures themselves. Studies report that they can safely and successfully do so with excellent results [13,14].
In Pakistan, the specialty of interventional nephrology is in its infancy. Vascular access care is fragmented, no fixed pathway exists for the creation of an AVF, and AVGs are too expensive. Patients do not have venous mapping procedures which would help maximize the success of AVF creation, and most nephrologists are un-involved in hemodialysis access planning. There is almost no published data about the state of interventional nephrology in Pakistan. In this study, we discuss the challenges faced in developing an interventional nephrology program at a tertiary care hospital affiliated with a medical university in Karachi, Pakistan. We will also present data from the center and provide possible solutions for the promotion and successful implementation of interventional nephrology in Pakistan.
Methods
We have established a new interventional nephrology program at Aga Khan University Hospital (AKUH) in Karachi, Pakistan. We encountered several challenges including turf issues, space and time allocation for the procedures, high costs of procedures, the dilemma of ownership of patients after the procedures, and referral issues. Some of them are described below.
Limitations of the study
Convincing the hospital management of the need for a new service: The initial challenge was to convince the hospital management of the need for a new service while other specialists (vascular surgeons, interventional radiologists) were performing these procedures in the hospital. A strong argument in favor of establishing an interventional nephrology service was that it would expedite AV access and dialysis catheter care for patients and make it more easily accessible. Furthermore, it would allow such procedures to be performed as an outpatient, hence potentially reducing costs by up to 30% compared to inpatient procedures and improve ESRD patient care.
Hospital credentialing: The management had reservations about the interventional nephrologist not being certified in radiology or surgery to perform the procedures. We presented the argument that since the interventionalist has been accredited by the American Society of Diagnostic and Interventional Nephrology (ASDIN) and has acquired ample training and experience in the USA, they can effectively perform the procedures. A proposal outlining the privileges of interventional nephrology was drafted which was eventually approved by the hospital privileges committee.
Turf battles: Previously, all vascular access management procedures were performed by vascular surgery and interventional radiology departments. Understandably, in the beginning, these specialties were not in favor of an interventional nephrology service at the hospital. After a series of meetings with these physicians to explain the interventional nephrology perspective, they agreed that this would be in the best interest of patients.
Equipment and space allocation: Interventional nephrology procedures require the use of a C-arm with fluoroscopy and Digital subtraction angiography and an ultrasound machine with linear probe and Doppler capability. This equipment is usually owned and used by interventional radiology and cardiology departments. It was evident very early on that these departments had little interest in sharing their equipment for procedures that were not of high priority to them.
An innovative solution was required and with the help of urology colleagues/leadership, we were able to modify the Siemens lithotripter C-arm machine and ultrasound for our procedures. A digital subtraction angiography program was added to the Siemens C-arm machine which was sufficient to perform the venoplasty and venogram procedures.
Another issue was about space allocation. Due to the busy schedules of cardiac catheterization laboratories and limited access to interventional radiology suites, it was difficult to schedule interventional nephrology procedures. Since establishing a dedicated laboratory required a large amount of capital, it was not an option. Therefore, we decided to perform the procedures in the lithotripsy suite till the patient volume increases and it is more feasible to establish a dedicated space.
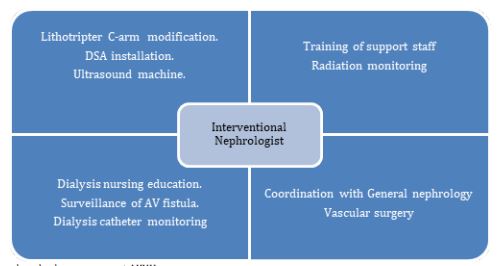
Training of the support staff: Our procedure team includes an operation theater (OT) technician with training and experience in sterile techniques and assistance during interventional procedures, a radiation and C-arm managing technician, a physician and nurse both certified in conscious sedation and the interventional nephrologist himself (Figure 1).
Figure 1: Interventional nephrology program at AKUH.
Lithotripsy support staff had experience in OT procedures and little training was needed to perform endovascular procedures. We used the available supplies in the hospital central distribution for interventional nephrology procedures including TDCs, guide wires, vascular sheaths, sutures, angioplasty balloons, etc.
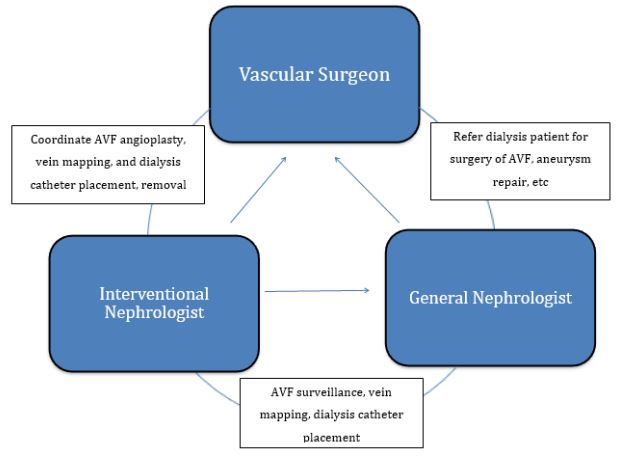
Since the role of dialysis unit nurses in vascular access management is crucial, we conducted a CME activity for them which comprised of lectures and hands-on sessions on how to effectively examine AVFs to identify signs of early dysfunction. We also described the kind of procedures performed by interventional nephrology and what they can expect from us. Finally, a coordination platform was set up between the interventional nephrologist, the general nephrologists, and vascular surgeons (Figure 2).
Figure 2: Dialysis access management with a multi-disciplinary team and vascular surgeons.
Results
Since December 2018 to October 2020, we have successfully placed 20 TDCs and performed 8 AVF venoplasty procedures. Since these procedures were performed as an outpatient, this helped save hospital beds for patients who warranted admission for various other medical necessities.
Typical catheter insertion by interventional nephrology service takes one hour from getting the patient pre-op to post-op, whereas venoplasty procedures take less than an hour. Patient monitoring is done for one hour post-procedure after which they are discharged home on the same day.
Even though we have performed few venoplasty procedures, the primary failure rates were <40%. Secondary patency at 3 months was 100% with no major side effects. An important issue was patients lost to follow-up. Out of the 8 venoplasty patients, only 1 followed up regularly thereafter.
Owing to the poor compliance with follow-up, we have only performed 4 venous mapping procedures, all of whom went on to obtain a successful AVF creation. We are also performing renal biopsies and plan on starting a peritoneal dialysis catheter placement program soon.
Currently, the interventional nephrologist allocates 70% of their time in practicing general nephrology and 30% to interventional nephrology practice. The overall nephrologist to patient ratio at our center is 1:20 (i.e. 5 nephrologists for 100 patients).
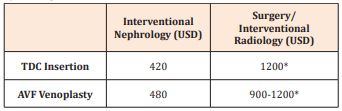
Vascular access procedures are costly and since most patients in our region pay out-of-pocket, the ability to schedule them as an outpatient has also helped decrease the cost burden. Table 1 shows the baseline costs incurred by patients undergoing TDC insertion or AVF venoplasty by interventional nephrology compared with other specialties.
Table 1: Estimates of cost differences (in USD) for Tunneled dialysis catheter (TDC) insertions and Arteriovenous fistula (AVF) venoplasty procedures performed by interventional nephrology compared to those
by other specialties.
*Estimates of the baseline costs incurred by patients admitted to the general ward of the hospital. Costs for semi-private and private room admissions are higher.
Discussion
Patient care in CKD is very fragmented when placed into the hands of other specialists. Interventional nephrology is a new subspecialty that addresses this problem by allowing nephrologists to get more involved in the diagnostic and procedural care of their patients.
In the year 2000, a group of American nephrologists established the American Society of Diagnostic and Interventional Nephrology (ASDIN) to provide the appropriate application of techniques that they have developed, and to improve patient care in nephrology [14]. It has been organizing an annual meeting since 2005 that allows the presentation and dissemination of the state-of-the-art interventional nephrology techniques and the latest research data.
Nephrologists from many countries who trained in the US under ASDIN-approved programs have established interventional nephrology programs in their respective countries [15]. A multidisciplinary approach is recommended for vascular access management involving the patient and their family, the nephrologist, the dialysis facility personnel, the surgeon, and the interventionalist; with the nephrologist playing a leadership role since they are the physicians who know the most about the patient, are experts in hemodialysis and have the deepest understanding of how vascular access impacts patient care [16]. In case of a vascular access dysfunction, a comprehensive evaluation by the interventional nephrologist is needed to direct the patient to the optimal treatment, which in some cases is surgical.
When we started the service at our center, our first obstacle was the assumption that we were stepping into other specialists’ fields, which is not the case as we are relieving other specialties of numerous examinations and interventions which may be of the utmost importance to us but are less of a priority for them. Vascular surgeons and interventional radiologists perform many types of procedures, and delays resulting from scheduling difficulties are avoided by interventional nephrology, which also contributes to better continuity of care. The new service at our center has the potential to enable timely and more focused care to be delivered to patients at reduced costs since we perform the same procedures in an outpatient instead of an inpatient setting. This is especially important for patients in our region since almost all are out-of-pocket and very little cost, if any, is covered by the government/insurance companies.
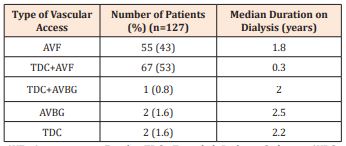
Running a dedicated interventional nephrology laboratory requires a large amount of capital. Since the subspecialty is in its infancy phase at our center and patient volume is low, it is currently not feasible to do so. We plan on establishing a dedicated laboratory in the future when the patient volume increases, and the cost-benefit ratio is more favorable. Our center currently has 3 dialysis units, all hospital-based, and has been unable to expand the units due to low patient volume, likely due to patients having to bear all the costs themselves. Vascular access management is expensive which also contributes to the low rate of patient follow-up; usually presenting when severe access dysfunction occurs. The current types of vascular accesses, along with the median years on dialysis of patients at our center are shown in Table 2. Unfortunately, over 50% of our patients use TDCs for dialysis, which are generally associated with a high risk of complications [17].
Table 2: Types of vascular access and median duration on dialysis at AKUH.
AVF: Arteriovenous Fistula; TDC: Tunneled Dialysis Catheter; AVBG: Arterio-Venous Bridge Graft
Vascular access care in Pakistan is not streamlined. The general practice involves patients being seen by the general nephrologist and dialysis nurse who refer them to a vascular surgeon if vascular access dysfunction is suspected. Frequently, due to scheduling difficulties or late referrals, a TDC needs to be placed instead of an AVF to support dialysis. The late evaluation also renders any salvage interventions of the vascular access less effective.
We have adopted a multidisciplinary approach at our center where the patient is seen by their general nephrologist and dialysis nurse and then referred to our service for interventional procedures based on dialysis treatment parameters or issues with dialysis access as evaluated by the nursing staff. These are also discussed at monthly meetings where we review reports of dialysis patients with the dialysis access nurse to determine the best management plan. The process has been streamlined after multiple educational lectures and hands-on seminars to educate the dialysis nurses and technicians. Another issue pertains to the ownership of dialysis patients once procedures are performed. In our opinion, this is best handled by the nephrology section.
Although to date we have performed few venoplasty procedures, our primary failure rates are comparable with those reported in the literature. (18) Due to poor patient follow-up, secondary patency rates beyond 3 months could not be determined for most patients. The results of TDC placement by our service seem promising. More patient data and better follow-up will enable us to determine the difference in outcomes of these procedures when performed by interventional nephrology compared to those performed by other specialties.
Some challenges we currently face and which are some limitation to this study:
● Lack of dedicated time and venue for vascular procedures
Performing procedures in the lithotripsy suite frequently leads to delays in management. In addition, there is one interventional nephrologist who performs these procedures, and shortage of time is a hindrance too.
● Inability to document venous mapping procedures
Pre-operative venous mapping has been shown to improve patency rates and decrease early failure rates for AVFs. (19) The current system at our center only allows a radiologist to generate a report in the electronic records system.
● Low patient compliance with regular surveillance of the AV access
The vascular access needs to be examined periodically to identify early signs of dysfunction. Even though patients are counseled sufficiently, many are lost to follow-up and present late for evaluation when salvage interventions are less effective, and a new vascular access needs to be created.
• The cost of dialysis catheters and angioplasty balloons have gone up due to hiking dollar rates.
Some solutions we would like to put forward are:
● Dedicated laboratory for interventional nephrology with daily procedures so that patients with clotted AVFs or malfunctioning catheters do not lose salvageable access and temporary catheter use in dialysis patients is reduced.
● A dedicated vascular access clinic started once a week to discuss vascular access creation plans with pre-ESRD patients beforehand to help eliminate future delays when the need arises. It would also allow routine examination of preexisting AVFs and AVGs at least once a month to identify signs of vascular access dysfunction so that timely interventions can be performed if needed.
● Multiple educational activities for dialysis nurses and technicians comprising CME and hands-on workshops.
● CME for nephrology faculty and trainees to increase awareness of these procedures
● Making AVF procedures outpatient only to control costs.
● Getting vascular surgeons on board as part of an interventional nephrology committee
● Conducting a study to report the improvement in patient care by starting this new service and using the data to convince the government to reduce duties and tariffs on interventional nephrology equipment.
● Developing a team effort with other specialists such as vascular surgeons, interventional radiologists, physicians, and cardiologists to ensure better patient outcomes and satisfaction.
● Patient advocacy is needed at multiple levels: at the community level to raise awareness about the importance of regular access surveillance; at the hospital administrators’ level to put the patients’ interests first; similar for governmental and non-governmental agencies and the public at large.
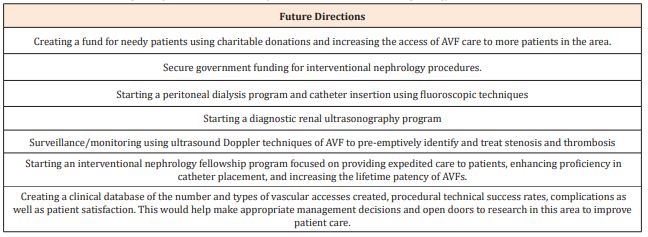
● In addition to the suggested solutions, we propose some future directions shown in Table 3.
Table 3: Future directions for improving vascular access management under interventional nephrology
Conclusion
In a country like Pakistan, where resources and surgical care are limited to bigger cities, interventional nephrology provides an opportunity for a well-trained nephrologist to provide ESRD patients with timely dialysis access and quicker solutions for access-related problems that subsequently occur. A program like ours can easily be established with help from other specialties and the support of the hospital administration.
Acknowledgements
None.
Conflicts of Interest
The authors have declared that there is no conflict of interest.
Funding
This is a non-funded study.
Ethical Approval
Approval from the Ethical Review Committee, AKUH was taken prior to conducting this study.
References
- Bill F, Foundation MG (2017) Global, regional, and national burden of chronic kidney disease, 1990 – 2017: a systematic analysis for the Global Burden of Disease Study 2017.
- Rizvi S, Anwar Naqvi S (1996) Renal Replacement Therapy in Pakistan. Saudi J Kidney Dis Transplant 7(4): 404–408.
- Efstratiadis G, Platsas I, Koukoudis P, Vergoulas G (2007) Interventional Nephrology: A new subspecialty of Nephrology. Hippokratia 11(1): 22–24.
- https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS
- Wasay M, Zaidi S, Khan M, Jooma R (2014) Non communicable diseases in pakistan: Burden, Challenges and way forward for health care authorities. J Pak Med Assoc 64(11): 1218–1219.
- Imtiaz S, Salman B, Qureshi R, Drohlia MF, Ahmad A (2018) A review of the epidemiology of chronic kidney disease in Pakistan: A global and regional perspective. Saudi J Kidney Dis Transpl 29(6): 1441–1451.
- Sachdeva B, Abreo K (2020) The History of Interventional Nephrology. Adv Chronic Kidney Dis 16(5): 302–308.
- Holmes JH, Howry DH, Posakony GJ, Cushman CR (1954) The ultrasonic visualization of soft tissue structures in the human body. Trans Am Clin Climatol Assoc 66: 208–225.
- O’Neill WC (2002) Seminars in nephrology. Introduction. Semin Nephrol 22(3): 181–182.
- Saad T (2004) Interventional Nephrology for Hemodialysis Vascular Access: Insight about an Evolving Branch. Saudi J Kidney Dis Transpl 15(3): 239–250.
- Arora P, Kausz AT, Obrador GT, Ruthazer R, Khan S, et al. (2000) Hospital utilization among chronic dialysis patients. J Am Soc Nephrol 11(4): 740–746.
- Mishler R, Sands JJ, Ofsthun NJ, Teng M, Schon D, et al. (2006) Dedicated outpatient vascular access center decreases hospitalization and missed outpatient dialysis treatments. Kidney Int 69(2): 393–398.
- Beathard GA, Terry Litchfield (2004) Effectiveness and safety of dialysis vascular access procedures performed by interventional nephrologists. Kidney Int 66(4): 1622–1632.
- Asif A, Byers P, Vieira CF, Roth D (2003) Developing a comprehensive diagnostic and interventional nephrology program at an academic center. Am J Kidney Dis 42(2): 229–233.
- Herrera-felix JP, Orias M (2020) Emergence of Interventional Nephrology at the International level. Adv Chronic Kidney Dis 16(5): 309–315.
- Beathard GA (2015) Kidney Research and Clinical Practice Role of interventional nephrology in the multidisciplinary approach to hemodialysis vascular access care. Kidney Res Clin Pract 34(3): 125–131.
- Lacson EJ, Lazarus JM, Himmelfarb J, Ikizler TA, Hakim RM (2007) Balancing Fistula First with Catheters Last. Am J Kidney Dis 50(3): 379–395.
- Cheung AK, Imrey PB, Alpers CE, Robbin ML, Radeva M, et al. (2017) Intimal Hyperplasia, Stenosis, and Arteriovenous Fistula Maturation Failure in the Hemodialysis Fistula Maturation Study. J Am Soc Nephrol 28(10): 3005–3013.
- Asif A, Ravani P, Roy-Chaudhury P, Spergel LM, Besarab A (2007) Vascular mapping techniques: advantages and disadvantages. J Nephrol 20(3): 299–303.