Updated Meta-Analysis Comparing FFR-Guided and Angiographic-Guided Intervention in Patients with Multivessel Coronary Artery Disease
Rohan M Prasad1*, Zulfiqar Q Baloch2, Robert Gumbita2, Zaheer Ahmed3, Heesoo Yoo1, Adolfo M Salazar1, Joel Cohn2
1Department of Internal Medicine, Michigan State University, USA
2Department of Cardiology, Sparrow Hospital, USA
3Department of Accident and Emergency Medicine, Royal Preston Hospital, UK
*Corresponding author: Rohan Madhu Prasad, Department of Internal Medicine, Michigan State University, Michigan, USA
Article History
Received: February 15, 2022 Accepted: March 03, 2022 Published: March 04, 2022
Citation: Prasad RM, Baloch ZQ, Gumbita R, et al. Updated Meta-Analysis Comparing FFR-Guided and Angiographic-Guided Intervention in Patients with Multivessel Coronary Artery Disease. Int J. Hert & Vasclr Syst. 2022;2(1):6‒10. DOI: 10.51626/ijhvs.2022.02.00007
Abstract
A new method to guide Percutaneous Coronary Interventions (PCI) and Coronary Artery Bypass Graft (CABG) interventions are by FFR, which is a measurement of the hemodynamic significance of coronary stenosis. We conducted an updated meta-analysis of all randomized controlled trials from inception to 5 December 2021 to compare studies that included patients who underwent FFR-guided PCI or CABG. The statistical analysis was performed using a random effect model to Calculate Risk Ratios (RR) and Mean Difference (MD) with 95% Confidence Intervals (CI). Five RCTs were included with a total of 2,288 patients and a median weighted follow-up period of 16.6 months. In this meta-analysis with a small sample size, there was no difference between FFR-guided and angiographic-guided interventions for the rates of MACE and all-cause mortality. Moreover, the analysis showed that FFR-guided was associated with insignificantly decreased rates of MI (RR 0.77, 95% CI 0.51-1.16, p=0.21, I2=18%) and the number of revascularizations (RR 0.82, 95% CI 0.64-1.06, p=0.12, I2=0%). Finally, the average number of stents used per patient significantly favored the FFR-guided group (MD -0.16, 95% CI -0.24 to -0.07, p=0.0003, I2=93%). In conclusion, although FFR-guided did not have any benefit in decreasing MACE or all-cause mortality, it was associated with improved outcomes of MI, the number of revascularizations, and the average number of stents.
Keywords: FFR; Fractional flow reserve; Angiographic; PCI; CABG; Multivessel; Meta-analysis; Randomized
Introduction
Traditionally, Percutaneous Coronary Interventions (PCI) and Coronary Artery Bypass Graft (CABG) procedures are done under the guidance of angiography. A newer method is using the value of using Fractional Flow Reserve (FFR) in the indication for intervention. FFR is measured by a coronary pressure wire that can be entered via the femoral or radial arteries [1]. FFR for a coronary artery is defined as the ratio of maximal achievable blood flow to the theorized maximal blood flow without any stenosis. To determine this ratio mean distal coronary artery pressure is compared to the mean aortic pressure during maximal hyperemia [2]. The cut-off value to indicate which lesions are hemodynamically significant is 0.80 [2]. Since FFR is a measure of two easily obtained pressure, it eliminates the operator-dependent evaluation of an angiographic image [2]. FFR also uses a lower dose of radiation and contrast medium as compared to coronary angiography [3]. Moreover, FFR accurately assesses the hemodynamic significance of coronary stenosis [1]. It is well known that CABG has short- and long-term advantages over PCI in patients with multivessel Coronary Artery Disease (CAD) [4]. Previous studies have demonstrated that FFR-guided PCI has beneficial outcomes in patients with multivessel CAD when compared to medical therapy and angiography-guided PCI [1,5-8]. Despite these studies, there is a gap of knowledge if FFR-guided CABG would still be preferred over FFR-guided PCI. In this updated meta-analysis, we aim to compare FFR-guided and angiographic-guided in studies that included patients with multivessel CAD that received PCI or CABG.
Methods
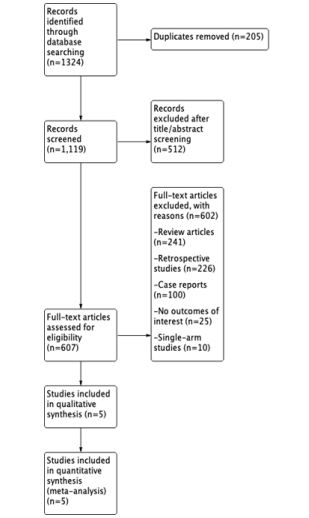
We conducted a comprehensive review of previous publications of all relevant studies from inception to 15 November 2021. We searched the electronic databases of PUBMED, EMBASE, COCHRANE, and Google scholar for RCTs. The search included the following keywords: “fractional flow reserve”, “FFR”, “angiographic”, “PCI”, “CABG”, “multivessel”, “randomized trial”. The inclusion criteria consisted of: (1) an RCT that compared FFR-guided and angiographic-guided interventions in patients with multivessel CAD, (2) the study reported more than 1 clinical or safety outcome, (3) human subjects, and (4) no restriction to language. Exclusion criteria were (1) follow-up data in < 90% of patients, (2) ongoing or irretrievable data, (3) no clinical outcome endpoint. This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Figure 1). Two authors (RMP and ZQB) independently reviewed the search results, extracted potential articles, and assessed their eligibility. The Cochrane Collaboration risk-of-bias tool was used by 2 different authors (RMP and ZQB) to assess the quality of the included studies.
Figure 1: The preferred reporting items for systematic reviews and meta-analyses (prisma) flow diagram.
The primary outcome was the rate of Major Adverse Cardiovascular Events (MACE). The secondary outcomes were the rates of all-cause mortality, myocardial infarctions, revascularizations, and the average number of stents used per patient. We also collected baseline characteristics of the study and patients. Statistical analysis was conducted using Review Manager (RevMan), version 5.4 (The Cochrane Collaboration, Copenhagen, Denmark). The Mantel-Haenszel random-effects models were used to estimate the Risk Ratio (RR) and Mean Difference (MD) along with the corresponding 95% Confidence Intervals (CI). Two-sided p values of less than 0.05 were considered statistically significant. I2 statistics were used to assess statistical heterogeneity.
Results
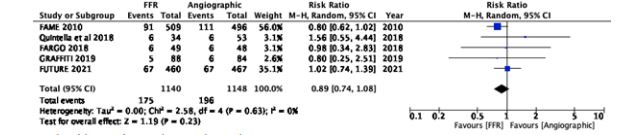
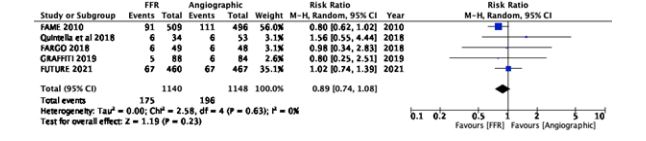
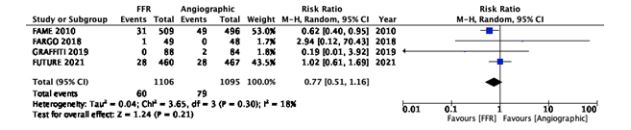
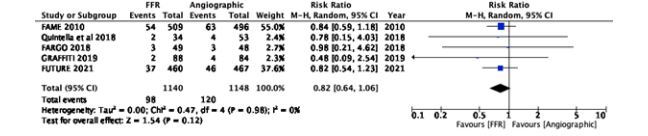
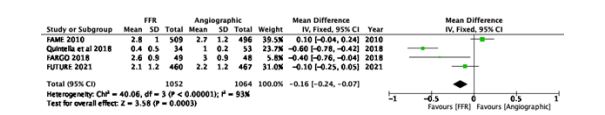
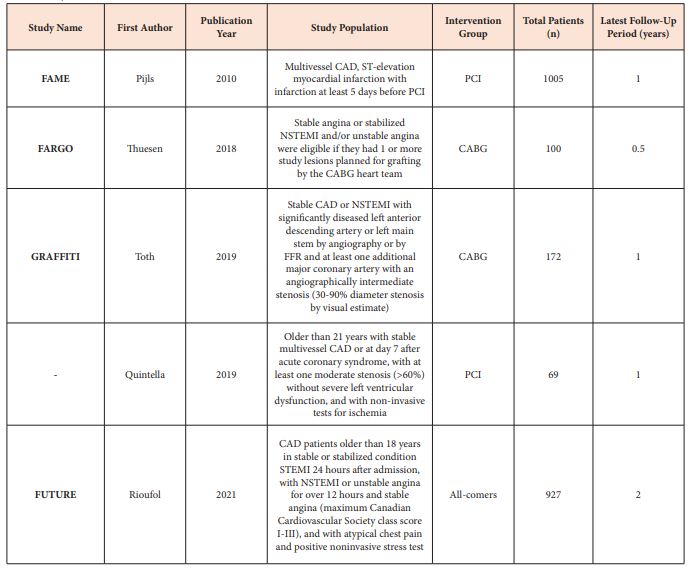
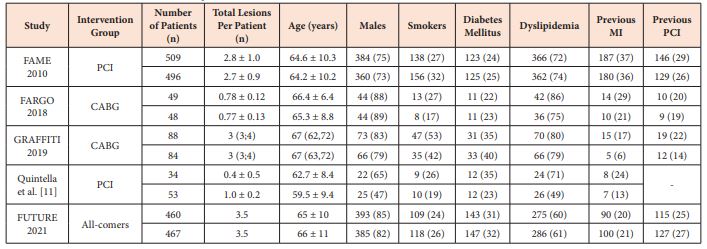
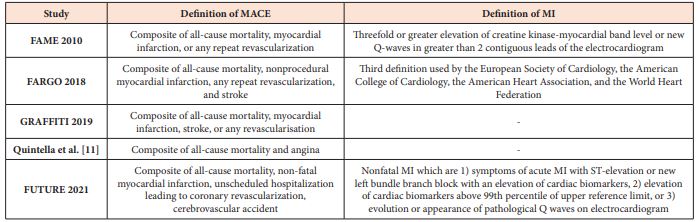
Five RCTs were included with a total of 2,288 patients and a median weighted follow-up period of 16.6 months (Figure 1) [9-13]. The characteristics of the included studies and patients are described in Tables 1 and 2. The definitions of the outcomes of MACE and MI for each of the included studies are reported in Table 3. There was no difference between FFR-guided and angiographic-guided interventions for the rates of MACE (RR 0.89, 95% CI 0.74-1.08, p=0.23, I2=0%) (Figure 2) and all-cause mortality (RR 1.22, 95% CI 0.53-2.78, p=0.64, I2=46%) (Figure 3). Moreover, the analysis showed that FFR-guided was associated with insignificantly decreased rates of MI (RR 0.77, 95% CI 0.51-1.16, p=0.21, I2=18%) (Figure 4) and the number of revascularizations (RR 0.82, 95% CI 0.64-1.06, p=0.12, I2=0%) (Figure 5). Finally, the average number of stents used in the intervention significantly favored the FFR-guided group (MD -0.16, 95% CI -0.24 to -0.07, p=0.0003, I2=93%) (Figure 6).
Figure 2: Forest plot of the rate of major adverse cardiovascular events.
Figure 3: Forest plot of the rate of all-cause mortality.
Figure 4: Forest plot of the rate of myocardial infarction.
Figure 5: Forest plot of the rate of revascularization.
Figure 6: Forest plot of the average number of stents per patient.
Table 1: Study characteristics of included randomized controlled trials.
Abbreviations: CABG: Coronary Artery Bypass Graft; CAD: Coronary Artery Disease; FFR: Fractional Flow Reserve; NSTEMI: Non-ST Elevation Myocardial Infarction; PCI: Percutaneous Coronary Intervention; STEMI: ST-Elevation Myocardial Infarction
Table 2: Baseline characteristics of included patients.
Values are reported as FFR | Angiographic. Units are reported as number (%), mean ± standard deviation, and median (IQR). Abbreviations: CABG, coronary artery bypass graft; FFR, fractional flow reserve; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Discussion
This meta-analysis with 2,288 patients and a median weighted follow-up period of 16.6 months illustrated that in patients with multivessel CAD there was no difference in the rates of MACE or all-cause mortality. However, FFR-guided was insignificantly associated with decreased MI and number of revascularizations as well as significantly lower average number of stents. Although our results showed that the FFR-guided method did not improve the short-term outcomes except for rates of MI, it did improve the procedural characteristics. Moreover, studies have evaluated other procedural outcomes, such as significantly less contrast agent, shorter hospital stay, fewer materials used, and a cheaper incremental health care cost. There were also similar procedural times between both the FFR-guided and angiographic-guided groups [9-11]. Additionally, FFR has been proposed to help decide the most appropriate revascularization method [12]. The FAME 3 trial demonstrated that FFR-guided PCI in patients with multivessel disease was not noninferior to CABG in regards to a composite of death, myocardial infarction, stroke, or repeat revascularization. Otherwise, this trial illustrated decreased median values of time to procedure, procedure duration, and length of hospital stay. Although this trial included a total of 1,500 patients, it was only conducted for 1 year and it has never been researched before [14].
The strengths of this meta-analysis include the short-term median weighted follow-up period of 16.6 months. The baseline characteristics of the patients in the included studies were grossly similar (Table 2). Additionally, based on the reported methods of the studies the technique of FFR was performed similarly.
Recently, Rioufol et al published the RCT FUTURE study that compared FFR-guided vs angiographic-guided in patients that received PCI or CABG. They showed that the FFR-guided arm did not result in a decreased risk of ischemic cardiovascular events, but did decrease the revascularization rates [14]. Of note, the initial RCTs included patients who exclusively received PCI [9,11] or CABG [10,12]. Therefore, FUTURE is the first study to randomly include all-comer patients. These findings were consistent with the previous studies, but the different inclusion criteria may have contributed to the level of heterogeneity seen in this meta-analysis. However, due to the limited number of studies in the current literature, we were unable to run a subgroup analysis to compare the different study populations of PCI, CABG, and all-comers. The other limitations of this meta-analysis were the small sample size and varying definitions of the clinical outcomes of MACE and MI (Table 3).
Table 3: Definitions of MACE and MI outcomes.
Abbreviations: MACE: Major Adverse Cardiovascular Events; MI: Myocardial Infarction
Conclusion
FFR-guided PCI or CABG has improved procedural characteristics and similar short-term outcomes. Further studies should be conducted to confirm these findings, evaluate the outcomes in a long-term setting, and directly compare FFR-guided PCI vs CABG.
References
- Xaplanteris P, Fournier S, Pijls NHJ, Fearon WF, Barbato E, et al. (2018) FAME 2 Investigators. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. N Engl J Med 379(3): 250-259.
- Tebaldi M, Campo G, Biscaglia S (2015) Fractional flow reserve: Current applications and overview of the available data. World J Clin Cases 3(8): 678-681.
- Ntalianis A, Trana C, Muller O, Mangiacapra F, Peace A, et al. (2010) Effective radiation dose, time, and contrast medium to measure fractional flow reserve. JACC Cardiovasc Interv 3(8): 821-827.
- Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, et al. (2018) Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet 391(10124): 939-948.
- Bech GJ, De Bruyne B, Pijls NH, de Muinck ED, Hoorntje JC, et al. (2001) Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 103(24): 2928-2934.
- Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, et al. (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360(3): 213-224.
- De Bruyne B, Fearon WF, Pijls NH, Barbato E, Tonino P, Piroth Z, et al.(2014) Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 371(13): 1208-1217.
- Layland J, Oldroyd KG, Curzen N, Sood A, Balachandran K, et al. (2015) Fractional flow reserve vs. angiography in guiding management to optimize outcomes in non-ST-segment elevation myocardial infarction: the British Heart Foundation FAMOUS-NSTEMI randomized trial. Eur Heart J 36(2): 100-111.
- Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, et al. (2010) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol 56(3): 177-184.
- Thuesen AL, Riber LP, Veien KT, Christiansen EH, Jensen SE, et al. (2018) Fractional Flow Reserve Versus Angiographically-Guided Coronary Artery Bypass Grafting. J Am Coll Cardiol 72(22):2732-2743.
- Quintella EF, Ferreira E, Azevedo VMP, Araujo DV, Sant’Anna FM, et al. (2019) Clinical Outcomes and Cost-Effectiveness Analysis of FFR Compared with Angiography in Multivessel Disease Patient. Arq Bras Cardiol 112(1): 40-47.
- Toth GG, De Bruyne B, Kala P, Ribichini FL, Casselman F, et al. (2019) Graft patency after FFR-guided versus angiography-guided coronary artery bypass grafting: the GRAFFITI trial. EuroIntervention 15(11): 999-1005.
- Rioufol G, Derimay F, Roubille F, Perret T, Motreff P, et al. (2021) Fractional Flow Reserve to Guide Treatment of Patients With Multivessel Coronary Artery Disease. J Am Coll Cardiol 78(19): 1875-1885.
- Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, et al. (2022) Fractional Flow Reserve-Guided PCI as Compared with Coronary Bypass Surgery. N Engl J Med 386(2): 128-137.