Chemodenervation with Botulinum Toxins for the treatment of Oromandibular dystonia
Mirza Sharyar Babar MBBS, MRCGP1, Javaria Mushtaq MD2, Muhammad Ismail Khalid Yousaf MD3
1Department of Family Medicine, The Saint Vincent Medical Center, UK
2Department of Histopathology, Rowan University, USA
3Department of Neurology, University of Louisville, USA
*Corresponding author: Javaria Mushtaq MD, Department of Histopathology, 210 Mullica Hill Road, Glassboro, NJ, USA
Article History
Received: January 11, 2022 Accepted: January 13, 2022 Published: January 17, 2022
Citation: Mirza Sharyar Babar MRCGP, Javaria Mushtaq MD, Khalid Yousaf MIMD. Chemodenervation with Botulinum Toxins for the treatment of Oromandibular dystonia. Int J Neuropsy Beh Sci. 2022;3(1):6‒7. DOI: 10.51626/ijnbs.2022.03.00023
Keywords
Oromandibular dystonia; Botulinum toxins; Movement disorders; Neurology
Opinion
Oromandibular dystonia (OMD) is a chronic lifelong disorder that usually causes repetitive or sustained dystonia movements of the mouth, jaw, and tongue or a combination of these movements [1]. The gross prevalence of OMD is estimated to be 9.8 per 100,000 individuals [2]. It is mostly seen in association with neurological and non-neurological disorders; however, isolated dystonias are uncommon. The dystonic movement involving OMD causes disfigurement of the face the patients are often stigmatized in society by their appearance. OMD is not only physically debilitating for the patients, but it also affects them psychologically. These patients tend to isolate themselves socially and are secondarily exposed to multiple psychiatric disorders, including anxiety, major depressive disorder, and suicide. Deficits of emotional processing are also reported in the patients suffering from OMD [3,4].
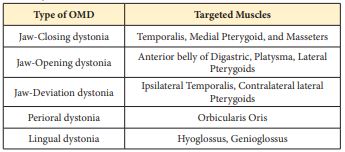
OMD is a type of focal dystonia that affects lower facial muscles. It is broadly classified into Jaw-closing dystonia, Jaw-opening dystonia, Jaw-deviating dystonia, Jaw-protrusion dystonia, Lingual dystonia, Perioral dystonia, or a combination of these dystonias. When blepharospasm (Involuntary close of the eyelids) is present in conjunction with OMD, it is known as Meigs Syndrome. Following muscles are commonly targeted in treating different types of dystonias.
OMD is frequently observed in conjunction with cervical dystonia as well [5,6]. OMD is diagnosed clinically, and there is no standard diagnostic criteria for this condition. Several pharmacological and non-pharmacological modalities are used for treating this condition, and the choice of treatment varies from patient to patient. Benzodiazepines, baclofen, zolpidem, tetrabenazines, dopaminergic agents (Levodopa), anticonvulsants, and carbamazepine are some of the oral medications used in the treatment of OMD. However, their use is limited due to the side effect profile, inadequate/subtherapeutic response, or high cost. Operative therapy, physiotherapy, and occupational therapy are also utilized to ease the symptoms of the patients to some extent [7].
Chemodenervation with Botulinum toxins (BoNT) are one of the safest and effective modalities for the treatment of oromandibular dystonia [8]. It involves injecting a potent bacterial neurotoxin that blocks the release of acetylcholine at the presynaptic terminal resulting in temporary denervation of the targeted skeletal muscle. Electromyography (EMG) is utilized for the better targeting of the involved muscle. EMG usage usually results in better outcomes and increased interval rate between subsequent injections [9].
There are four most commonly used commercial preparation of botulinum toxins available in the market Dysport®, MyoBloc/NeuroBloc®, Xeomin®, and Botox®, and each of them differ in efficacy, potency, and dosage in treating dystonias [10]. Currently, there is a level C recommendation for Abo-BoNT and Ona-BoNT. Rima-BoNT B and Inco-BoNT A carry level U recommendations according to class I clinical practice guidelines [11].
Table 1: Types of Oromandibular Dystonias and the Muscle(s) Targeted for the BoNT injections
In our practice, the OMD is best treated with botulinum toxins. As this procedure is technique-dependent excellent results can be obtained in experienced hands. Familiarity with the anatomy, knowledge about accurate dosing, proper injection technique, and utilization of the EMG can give remarkable results with minimum or no side effects. Some of the adverse effects that can be seen in the patients are injection site swelling/pain, dysarthria, dysphagia, dizziness, skin rashes, dry mouth, dysphonia, problems in chewing solid foods, etc. Dysphagia is one of the severe complications that can occur while injecting for lingual dystonia, which is by far the most complicated dystonia to treat [12]. However, careful dose titration and EMG utilization can minimize the temporary adverse effects.
Long-term management of oromandibular dystonia with chemodenervation utilizing botulinum toxins is a safe and effective treatment. Due to the rarity of the conditions and inadequate trials, the data lacks in establishing the long-term effects of toxins. Prospective clinical trials or randomized clinical trials (RCT) can establish the best treatment strategies for the treatment of OMD.
Funding
Authors declare no specific grant for this research from any funding agency in public, commercial or not-for-profit sectors.
Conflict of Interest
No conflict. All authors agree to the final draft of the manuscript.
References
- Ameer MA, Bhatti D (2021) Chemodenervation for Oromandibular Dystonia Utilizing Botulinum Toxins. Cureus 13(10): e18425.
- Yoshida K (2021) Prevalence and incidence of oromandibular dystonia: an oral and maxillofacial surgery service–based study. Clin Oral Investig 25(10): 5755–5764.
- Gharzai L, Harney J, Higgins S, High R, Xu L, et al. (2020) Alarming levels of stigma toward generalized dystonia: A cross-cultural comparison. Clin Park Relat Disord 3: 100059.
- Zurowski M, McDonald WM, Fox S, Marsh L (2013) Psychiatric comorbidities in dystonia: Emerging concepts. Mov Disord 28(7): 914–920.
- Muhammad Atif Ameer, Danish Bhatti (2020) Chemodnervation For Cervical Dystonia: A Clinical Review. Khyber Med Univ J 12(3).
- Pandey S, Sharma S (2017) Meige’s syndrome: History, epidemiology, clinical features, pathogenesis and treatment. J Neurol Sci 372: 162–170.
- Cloud LJ, Jinnah H (2010) Treatment strategies for dystonia. Expert Opin Pharmacother 11(1): 5–15.
- Ameer MA, Syed N, Bertoni J, Hellman A, Torres-Russotto D, et al. (2020) Chemo-denervation of Oromandibular Dystonia with Botulinum toxins: Five-year experience (2794). Neurology 94(15): 2794.
- Jankovic J (2004) Botulinum toxin in clinical practice. J Neurol Neurosurg Psychiatry 75(7): 951–957.
- Bhidayasiri R, Cardoso F, Truong DD (2006) Botulinum toxin in blepharospasm and oromandibular dystonia: comparing different botulinum toxin preparations. Eur J Neurol 13: 21–29.
- Persaud R, Garas G, Silva S, Stamatoglou C, Chatrath P, et al. (2013) An evidence-based review of botulinum toxin (Botox) applications in non-cosmetic head and neck conditions. JRSM Short Rep 4(2): 1–9.
- Comella CL (2018) Systematic review of botulinum toxin treatment for oromandibular dystonia. Toxicon 147: 96–99.