Atypical Posterior Reversible Encephalopathy Syndrome (PRES) with Strokes as a Presentation of Neuropsychiatric Systemic Lupus Erythematosus (NPSLE)
Muhammad Ismail Khalid Yousaf1*, Muhammad Atif Ameer2, Tracy M Ander DO1
1Department of Neurology, University of Louisville, USA
2Department of Medicine, University Hospital Bristol Weston NHS Foundation Trust, UK
*Corresponding author: Muhammad Ismail Khalid Yousaf, Department of Neurology, University of Louisville, Academic Offices, 500 South Preston St. HSC-A Bldg, Suite 113 Louisville, KY 40202, USA
Article History
Received: December 24, 2021 Accepted: December 31, 2021 Published: January 03, 2022
Citation: Yousaf MIK, Ameer MA, Ander TMDO. Atypical Posterior Reversible Encephalopathy Syndrome (PRES) with Strokes as a Presentation of Neuropsychiatric Systemic Lupus Erythematosus (NPSLE). Int J Neuropsy Beh Sci. 2022;3(1):105‒107. DOI: 10.51626/ijnbs.2022.03.00022
Abstract
Posterior reversible encephalopathy syndrome (PRES) is a rare clinical and radiological syndrome that can manifest as altered mental status, seizures, visual problems, and headaches. It is diagnosed by visualizing vasogenic edematous changes in brain scans. More often occipital and parietal lobes are involved, severe/atypical PRES can involve bilateral cerebral hemispheres, cerebellum, and brainstem as well. Patients with autoimmune disorders and hypertension can present with PRES. Although cerebrospinal fluid (CSF) findings in PRES are less studied, few studies show an association between radiological severity and CSF findings in PRES patients.
Keywords: Neurology; Posterior reversible encephalopathy syndrome (PRES); Neuropsychiatric systemic lupus erythematosus (NPSLE); Steroids
Abbreviations
PRES: Posterior Reversible Encephalopathy Syndrome; CSF: Cerebrospinal Fluid; SLE: Systemic Lupus Erythematosus; MRI W/WO: Magnetic Resonance Imaging with and without Contrast; CT: Computerized Tomography; ESR: Erythrocyte Sedimentation Rate; ACD: Albumino-Cytological Dissociation; NPSLE: Neuropsychiatric Systemic Lupus Erythematous; igM: Immunoglobulin M
Introduction
We present a case of atypical PRES with strokes in a patient with a known diagnosis of systemic lupus erythematosus. Ellis CA et al. [1] article on implications of high protein and pleocytosis in CSF of PRES patients was clinical in a case which we recently encountered.
Case Report
57-year-old female with a known past medical history of hypertension and rheumatological disorders, including systemic lupus erythematosus (SLE), Raynaud syndrome, and rheumatoid arthritis, presented with altered mental status and hypertensive emergency (blood pressure 205/110 mm hg). The patient was afebrile with leukopenia (3.1 x 10(3)/uL) and thrombocytopenia (137 x 10(3)/uL). Renal and liver function tests were within normal limits. Her medications include daily lisinopril 10 mg, amlodipine 10 mg, hydrochlorothiazide 25 mg, prednisone 5 mg, hydroxychloroquine 200 mg, and carvedilol 25 mg twice a day. She was non-compliant with her blood pressure medications as per her family. The family also denied seizures, falls, and recent infections.
No lateralizing findings were noticed, including cranial nerve deficits, limb weakness, and ataxia. She was only alert and oriented to herself. At home, she was able to walk and do her chores including bills and groceries [2].
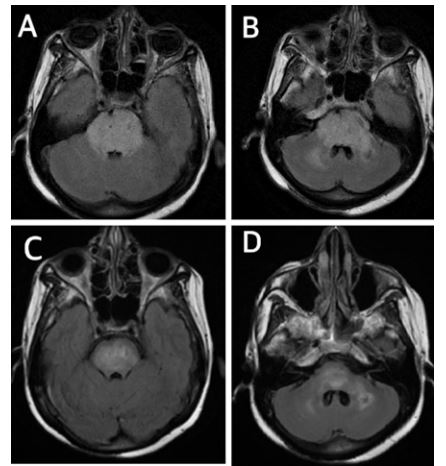
Her brain computerized tomography (CT) scan showed bilateral sulcal effacement with edematous changes of the pons and bilateral thalami. Chronic left cerebellum infarct was also seen. Her brain Magnetic Resonance Imaging with and without contrast (MRI W/WO) showed T2 flair hyperintensities in bilateral cerebral hemispheres and throughout the brainstem (Figure 1A & B). There was no abnormal post-contrast enhancement in any part of the brain. Small acute diffusion restriction in the left temporal lobe confirmed a small stroke. An ophthalmology fundoscopy exam did not reveal papilledema and hydroxychloroquine toxicity; however, the report suggested bilateral retinal hemorrhages.
We obtained cerebrospinal fluid (CSF) to rule out central nervous system infection and any inflammatory process. The lumbar puncture had an opening pressure of 370 mm H2O. CSF labs showed albumino-cytological dissociation (ACD) with protein 90 mg/dL (normal < 45 mg/dL), 3 cells/µL nucleated cells (normal < 5 cells/µL), and negative CSF culture. The meningoencephalitis panel was negative except for positive Cytomegalovirus (CMV) Immunoglobulin G (IgG). CT chest, abdomen, and pelvis did not reveal any malignancy. Blood cultures turned out negative. The autoimmune panel later was also negative. No oligoclonal bands were present.
Due to her rheumatological history, negative acute infectious workup, and MRI’s impressive and uncanny T2 flair findings, especially in the brainstem, our top diagnosis was atypical PRES as a presentation of Neuropsychiatric systemic lupus erythematous (NPSLE) [3]. While she was on tight blood pressure control through nicardipine drip (gradual 25% decrease in systolic blood pressure over couple of hours), she was also started on hypertonic 3% saline to counter against the widespread edema in the brainstem (Figure 1- A and B). After stable brain computerized tomography (CT) scans for two consecutive days, we stopped the hypertonic solution. However, the patient was still waxing and waning in mental status. Electroencephalogram (EEG) showed poorly sustained 6-7 Hz activity, suggesting overall encephalopathy.
On the 3rd day, we started her on high-dose methylprednisolone (1 gm x 5 days) with continued blood pressure control in the intensive care unit setting.
Discussion
We found Ellis CA et al. [1] article was helpful in interpreting our findings. Their study concluded that ACD is a common finding in PRES and CSF protein elevation was significantly associated with the severity of vasogenic edema visualized on MRI, but not with seizures- as also seen in our patient. Although the article suggested patients with CSF pleocytosis showed a higher incidence of infarcts and hemorrhage in the brain, the patient we treated did not have CSF pleocytosis yet had repeated small infarcts.
Our rationale for inpatient strokes, despite blood pressure control, no evidence of atrial fibrillation, and no thromboembolic source in heart and neck vessels (confirmed through transthoracic echo and CT angiography brain and neck respectively), were:
a. Persistent hypertension- patient blood pressure was gradually normalized over days.
b. Vasculitis caused by PRES/NPSLE (2). Inflammatory markers were positive for inflammation as: Erythrocyte Sedimentation Rate (ESR) of 113 mm/Hr. (normal < 20 mm/Hr.), C-reactive protein of 8.28 mg/liter (normal < 5 mg/liter), IgG 2197 mg/dL (normal range 750-1560 mg/dL), and serum protein electrophoresis gamma globulin 2.27 g/dL (normal 0.73- 2 g/dL).
c. Mild hypercoagulable state secondary to autoimmune disorders- patient’s phosphatidylserine Immunoglobulin M (igM) was >100 U/mL (normal < 100 U/mL).
Progressively, she was back to her baseline mental status, which her daughters were monitoring. After eight days of medical management, a repeat MRI W/WO showed decreased T2 flair hyperintensities, especially in the brainstem (Figure 1C & D), but with four new bilateral cerebral hemispheres acute/subacute infarcts. Stable bilateral cerebral microhemorrhages as seen in gradient echo sequences (GRE) previously as well. Low dose aspirin along with statin was started.
Figure 1: A & B On admission MRI Brain T2 flair show hyperintensities in brainstem consistent with vasogenic edema.
C & D: Improved vasogenic edema in brainstem on 8th day after 5 days of high dose steroids.
All our acute infectious workup was negative. Pro-inflammatory pathophysiology of atypical PRES in this patient is relevant due to high CSF protein.
Conclusion
In encephalopathic patients with high blood pressure and autoimmune history, especially SLE, it is essential to rule out PRES through MRI Brain promptly. If positive, it is critical to categorize the severity of radiological and CSF findings to preempt vascular complications, i.e., stroke and hemorrhage [4]. PRES can present as a variant of NPSLE [3,5] Future studies should focus on the antiplatelet therapy role in such cases. Blood pressure control and timely high-dose steroid administration in patients like ours could be “brain saving.”
Conflict of Interest
No conflict. All authors agree to the final draft of the manuscript.
Funding
Authors declare no specific grant for this research from any funding agency in public, commercial or not-for-profit sectors.
Consent
Written consent was given by patient to use images and information.
Acknowledgment
None.
References
- Ellis CA, Mcclelland AC, Mohan S, Kuo E, Kasner SE, et al. (2018) Cerebrospinal Fluid in Posterior Reversible Encephalopathy Syndrome: Implications of Elevated Protein and Pleocytosis. The Neurohospitalist 9(2): 58–64.
- Shaharir S, Remli R, Marwan A, Said M, Kong N (2013) Posterior reversible encephalopathy syndrome in systemic lupus erythematosus: pooled analysis of the literature reviews and report of six new cases. Lupus 22(5): 492–496.
- Ho C, Mok C (2019) Posterior reversible encephalopathy syndrome as a neuropsychiatric manifestation of systemic lupus erythematosus. Hong Kong Medical Journal 25(5): 410-412.
- Schweitzer AD, Parikh NS, Askin G, Nemade A, Lyo J, et al. (2017) Imaging characteristics associated with clinical outcomes in posterior reversible encephalopathy syndrome. Neuroradiology 59(4): 379–86.
- Liu B, Zhang X, Zhang F-C, Yao Y, Zhou R-Z, et al. (2012) Posterior reversible encephalopathy syndrome could be an underestimated variant of “reversible neurological deficits” in Systemic Lupus Erythematosus. BMC Neurology 12(1): 152.