Surgery Option for Treatment of Sacroiliitis
Adnan A Faraj*
Consultant orthopaedic surgeon, Scarborough Hospital, UK
*Corresponding author: Adnan A Faraj, orthopaedic surgeon, Scarborough General hospital, Woodland Drive, Scarborough, UK
Article History
Received: May 03, 2021 Accepted: May 14, 2021 Published: May 21, 2021
Citation: Faraj AA. Surgery Option for Treatment of Sacroiliitis. Int J. Orth & Trauma. 2021;1(1):05‒07. DOI: 10.51626/ijot.2021.01.00002
Abstract
The Sacroiliac joint pain can be disabling. Non-surgical treatment includes physiotherapy (structured core and pelvic muscle flexibility and strengthening) in addition to different types of analgesia. Surgical treatment is reserved for severe pain not responding to conservative treatment. Surgical fusion of sacroiliac joint is an option. The procedure can be performed open or through minimally invasive surgery. The latter is shown to have lower morbidity and earlier recovery than traditional open approaches. The evidence for surgery (open or through minicam invasive approach)s, is still not well evidenced in literature, however, what is published shows a good pain relief following surgery.
Introduction
Sacroiliac joint fusion is suitable as a surgical treatment for degenerative sacroiliitis, inflamed sacroiliac joint dysfunction, iatrogenic instability of the sacroiliac joint, osteitis condensans ilii (OCI), traumatic fracture dislocation of the pelvis, and other causes of sacroiliitis. Sacroiliac joint fusion need to be performed as an adjunct to sacrectomy or partial sacrectomy related to tumors involving the sacrum; or when multisegment spinal constructs extend to the sacrum/ilium. At this time, however, there is no evidence-based guideline or position statement regarding sacroiliac spinal fusion procedures from the American Association of Neurological Surgeons (AANS), the American Academy of Orthopaedic Surgeons (AAOS), and the American Pain Society (APS) to support the use of sacroiliac joint fusion in treating mechanical low back pain due to sacroiliac joint syndrome and sacral insufficiency fractures.
Identifying the Source of Pain
Methods of confirming the sacroiliac joint as a pain source have been extensively studied and reported in the literature. After confirmation of the origin of the pain by positive local anesthetic blocks, chronic sacroiliac joint pain is usually managed with a combination of medication, physical therapies, and injections.
Surgical Options for Sacroiliac Joint Arthtitis
Electronic databases and reference lists of key articles were searched to identify studies evaluating surgical management of chronic sacroiliac joint pain after failed conservative management. Patients with moderate to severe sacroiliitis who do not respond to conservative sacroiliitis treatments have two surgical options; denervation of the joint and fusion of the sacroiliac joint [1]. In a systematic review [1]; metaanalysis, eleven articles concerning fusion, and denervation of the sacroiliac joint, were found. Six studies evaluated fusion for sacroiliac joint pain (n = 95 patients). Five studies evaluated denervation for sacroiliac joint pain (n = 68 patients). All studies were case series evaluating a single treatment. No cohort studies comparing one treatment to the other in the same patient population was identified, making statements regarding relative efficacy impossible. Further, follow-up times for denervation studies (6–12 months) were much shorter than fusion studies (17–69 months). All studies involved subjects who had failed other conservative management. A diagnosis of sacroiliac joint pain in all studies was confirmed by injection. Prior to their denervation treatment all patients in the denervation cohort underwent physical therapy and medical therapy. Some patients also underwent injection therapy or had previous back surgery. Many patients in the fusion cohort had previously undergone lumbar fusion and other types of back surgery. The majority of subjects report satisfaction after either treatment. Both treatments appear to demonstrate improvement in outcomes from pre to posttreatment during their follow-up period. The majority of patients report satisfaction after both treatments however rates of complications were higher among fusion studies (13.7%) compared to denervation studies (7.3%). Only fusion studies reported infections (5.3%). No infections were reported among denervation patients. The evidence for all findings were very low to low; therefore, the relative efficacy or safety of one treatment over another could not be established.
Complication rates and infection rates were higher among those undergoing fusion compared to those undergoing denervation.
The existing literature is limited to case series. No studies were identified that compared treatments in the same patient population. Given these limitations, pooled rates from these studies must be taken with caution. The open fusion studies reported poorer results and higher complication rates than the percutaneous studies. However, the concept of ‘fusion’ of the sacroiliac joint after percutaneous fixation with hollow screws or cages filled with bone-graft substitute was based on the absence of loosening on plain x-rays or confirmation of trabecular continuity across the implants on CT scanning. Also, many of the patients in the fusion series had undergone previous spinal surgery, suggesting that a positive response to sacroiliac blocks does not predict successful pain relief after sacroiliac fusion in patients with chronic pain syndromes [2-12].
Good outcome measure in a study was obtained in only 48% of patients undergoing sacroiliac joint fusion. The patients with successful 1-year outcomes retain significantly improved function and reduced pain levels, and the 1-year outcomes were sustained 23 years after surgery compared with the subgroup of patients with unsuccessful 1-year outcomes (28 %) [13].
Techniques for Sacroiliac Joint Fusion
The variation in the percentage of good outcome seem to be be related to the technique used in the fusion. The current review article pruses through different techniques used for chronic sacroiliac pain, the paper does not study acute sacroiliac joint disruption treated with iliosacral screws.
Open Sacroiliac Joint Fusion
Anterior or posterior sacroiliac joint fusion, using bone graft with or without fixation, is an invasive procedure, with relatively poor outcome compared to percutaneous fusion. The bone graft used can be taken from the iliac bone, or elsewhere. In a study, eleven consecutive patients with persistent late pain following iliosacral screw fixation were managed with fibular bone grafting of the SI joint. Eight patients were pain free and returned to their work. The remaining three patients were having persistent-localized pain, but they were able to manage their daily activities. There were neither intraoperative complications nor postoperative wound infection. The authors concluded in this paper that fibular graft is feasible and apparently effective choice for SI joint fusion [14]. However, the author fails to appreciate donor site morbidity, additionally there were three patients with persistent postoperative pain.
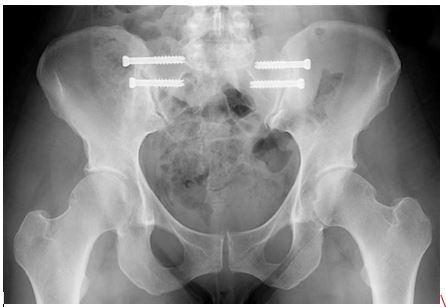
Minimal invasive surgery for Treatment of Sacroiliitis: New generation of implants and minimally invasive percutaneous techniques has been advocated without scientific long-term outcome measure publication in peer review journal [Figure 1 & 2]. It is claimed that this new technique using radiographic guidance during the procedure gives the enormous advantage of decreasing blood loss, reducing operative time, and preventing extensive surgery [15]. In a study, the overall fusion rate after percutaneous sacroiliac joint fusion using bone morphogetic protein filled cages for positive responders of sacrioilitis was 89% (17/19 joints) in 13 patients (19 joints). However the outcome measure used was visual pain analogue, and one patient was revised to an open arthrodesis secondary to non-union and persistent pain [15].
Figure 1: Technique using percutaneous sacroiliac joint fusion.
Figure 2: Demonstrating the metallic pegs inserted in to the sacroiliac joint.
In another study, using computerized tomography (CT) guided percutaneous sacroiliac joint fusion, on 11 patients; pain was used as the only outcome measure, 11 out of 17 patients had significant pain relief; which was statistically significant [16].
In a study on 15 consecutive patient undergone percutaneous sacroiliac fusion using hollow modular anchorage screws filled with demineralised bone matrix, the mean short form-36 scores improved from 37(23 to 51) to 80(67 to 92) for physical function and from 53(34 to 73) to 86(70 to 98) for general health (p = 0.037 and the mean Majeed’s score improved from 37(18 to 54) pre-operatively to 79 (63 to 96) post-operatively (p = 0.014). There were 13 good to excellent results. The remaining two patients improved in short form-36 from a mean of 29(26 to 35) to 48(44 to 52). Their persistent pain was probably due to concurrent lumbar pathology. The authors conclude that percutaneous hollow modular anchorage screws are a satisfactory method of achieving sacroiliac fusion [17]. Percutaneous sacroiliac joint fusion can also be used for septic sacroiliitis [18].
Although the fusion the sacroiliac joint can be done without fixation [19], the trend is to use Metallic fixation of the sacroiliac joint:
Types of Implants used Specifically for Sacroiliac
Joint Fusion
There are two types, Smooth or threaded metallic bone fastener, both are approved by Food and Drug Administration as Class II devices. The system consists of a series of metallic (titanium), porous plasma spray coated rods, intended for surgical implantation within the bone to create fixation. The system includes 4.0 mm and 7.0 mm diameter fusion rods, which range in length from 30 mm to 70 mm. Another device, the SImmetry™ Sacroiliac Joint Fusion System (Modification) received special 510(k) clearance on March 23, 2011 (K110512) as substantially equivalent to a predicate device cleared under K10290. The Simmetry™ Sacroiliac Joint Fusion System consists of cannulated screws available in titanium having diameters ranging from 6.5mm-12.5mm, lengths of 30mm-70mm, and titanium washers are available for the 6.5 mm diameter screws. Both systems are intended for sacroiliac joint fusion for conditions including sacroiliac joint disruptions and degenerative sacroiliitis [20-23].
Conclusion
There is no doubt that the future option for positively responding sacroiliitis to local anaesthetics and when conservative treatment fails to relieve pain, percutaneous approach using fixation and bone morphogenic protein or equivalent material will be the way forwards. Randomized, controlled trials comparing sacroiliac joint fusion to standard treatments are needed to determine the impact on health outcomes and long-term efficacy.
References
- Bryan Ashman, Daniel C Norvell, Jeffrey T Hermsmeyer (2010) Chronic sacroiliac joint pain: fusion versus denervation as treatment options. Evid Based Spine Care J 1(3): 35–44. HYPERLINK “http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Norvell%20DC%5Bauth%5D”
- Wise C L, Dall B E (2008) Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 21(8): 579–584.
- Schutz U, Grob D (2006) Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg 72: 296–308.
- Al Khayer A, Hegarty J, Hahn D, M P Grevitt (2008) Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech 21(5): 359–363.
- Buchowski JM, Kebaish KM, Sinkov V, DB Cohen, AN Sieber, et al (2005) Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J 5(5): 520-528.
- Burnham RS, Yasui Y (2007) An alternate method of radiofrequency neurotomy of the sacroiliac joint: a pilot study of the effect on pain, function, and satisfaction. Reg Anesth Pain Med 32(1): 12–19.
- Cohen SP, Hurley RW, Buckenmaier CC, Kurihara C, Morlando B, et al (2008). Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology 109(2): 279–288.
- Cohen S P, Abdi S (2003) Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med 28(2): 113–119.
- Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph NJ (2006) Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med 7(5): 429–434.
- Khurana A, Guha AR, Mohanty K, Ahuja S (2009) Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br 91(5): 627–631.
- Yin W, Willard F, Carreiro J, Dreyfuss P (2003) Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine 28(20): 2419–2425.
- Waisbrod H, Krainick JU, Gerbershagen HU (1987) Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg 106(4): 238–240.
- Kibsgård TJ, Røise O, Sudmann E, Stuge B (2012) Pelvic joint fusions in patients with chronic pelvic girdle pain: a 23-year follow-up. Eur Spine J 22(4): 871-877.
- Ebraheim NA, Ramineni SK, Alla SR, Ebraheim M (2010) Sacroiliac joint fusion with fibular bone graft in patients with failed percutaneous iliosacral screw fixation. J Trauma 69(5): 1226-1229.
- Phillips FM, Garfin SR (2011) Minimally invasive sacroiliac joint fusion. Orthopedics 34(8): 600-601.
- Ziran BH, Heckman D, Smith WR (2007) CT-guided stabilization for chronic sacroiliac pain: a preliminary report. J Trauma 63(1): 90-96.
- Khurana A, Guha AR, Mohanty K, Ahuja S (2009) Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br 91(5): 627-630.
- Giannoudis PV, Tsiridis E (2007) A minimally invasive technique for the treatment of pyogenic sacroiliitis. J Bone Joint Surg Br 89(1): 112-114.
- Giannikas KA, Khan AM, Karski MT, Maxwell HA (2004) Sacroiliac joint fusion for chronic pain: a simple technique avoiding the use of metalwork. Eur Spine J 13(3): 253-256.
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, et al. (2009) Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976) 34(10): 1066-1077.
- http://www.accessdata.fda.gov/cdrh_docs/pdf11/K110838.pdf
- http://www.accessdata.fda.gov/cdrh_docs/pdf11/K110512.pdf
- Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 17(6): 794-819.