Eosinophilic Gastroenteritis: A Rare Digestive Disorder
Haythem Yacoub*, Hela Kchir, Hajer Hassine, Nadia Maamouri
Gastroenterology B department, La Rabta Hospital, Tunisia
*Corresponding author: Haythem Yacoub, Gastroenterology B department, La Rabta Hospital, Tunis, Tunisia
Article History
Received: July 24, 2021 Accepted: August 10, 2021 Published: August 13, 2021
Citation: Yacoub H, Kchir H, Hassine H, et al. Eosinophilic Gastroenteritis: A Rare Digestive Disorder. Int. Jr. Infect Dis & Epidemlgy. 2021;2(2):36‒38. DOI: 10.51626/ijide.2021.02.00007
Abstract
Eosinophilic gastroenteritis is a rare digestive disorder in children and adults characterized by eosinophilic infiltration of the gastrointestinal tract. The symptoms are nonspecific and vary, depending on the site and layer of the bowel wall infiltrated by eosinophils. Unlike eosinophilic oesophagitis, the management of eosinophilic gastroenteritis is not consensual. The course of this pathology is variable and spontaneous remission is possible. In some patients, recurrent symptoms have been reported after corticosteroid interruption.
Keywords : Eosinophilic gastroenteritis ; Eosinophils ; Stomach ; Intestines ; Colon
Introduction
Eosinophilic gastroenteritis (EGE) is a rare digestive disorder that was first described in 1937 by Kaijser. This entity is a part of eosinophilic gastrointestinal disorders including eosinophilic esophagitis, eosinophilic gastroenteritis, and eosinophilic colitis [1]. Among these disorders, EGE is a heterogeneous disease characterized by eosinophilic infiltration of the gastrointestinal tract.
Unlike eosinophilic esophagitis, whose incidence is clearly increasing, EGE is still a rare but underestimated pathology due to the varied and non-specific symptoms it causes.
Its prevalence is estimated about 8.4/100,000 inhabitants in the United States [2]. It affects both adults and infants with peak prevalence around 30 years. Male seem to be more affected by EGE.
Methods
The bibliographic search was conducted using the following sites: Cochrane and Pubmed. The key words used were: eosinophilic gastroenteritis, eosinophilic esophagitis, and eosinophilic gastrointestinal diseases.
Definition and Differential Diagnosis
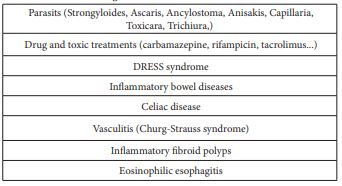
EGE is defined as histological eosinophilic infiltration of one or more components of the digestive wall greater than 20 eosinophils per field at high power field (HPF) (× 400) [3,4]. This infiltration can affect one or more segments of the gastrointestinal tract. Eosinophils are recruited in response to several stimuli such as infections including parasites, nonspecific tissue injuries, and allergens. The differential diagnosis is mainly related to parasitic infections, toxic causes, vasculitis and inflammatory bowel diseases. The main differential diagnoses are summarized in Table 1.
Table 1: Differential diagnoses of EGE.
Pathophysiology
Eosinophils play an important role in the pathogenesis of certain inflammatory diseases and allergic reactions. They also play a major role in protecting the organism from parasitic infections. Except in the esophagus, where their presence is pathological, eosinophils are found in the mucosa of the gastrointestinal tract. Therefore, a microscopic examination that reveals >15 eosinophils /HPF has been set as the threshold for the diagnoses of EGE. Normal eosinophils count varies based on the anatomic site of the gastrointestinal tract [5]. The number of eosinophils gradually increases from the stomach to the terminal ileum and right colon.
The exact pathophysiology of EGE is still not well understood. Allergy seems to play an important role, as the prevalence of food allergies in patients with EGE is high. Various food allergens may cause inflammation in the gastrointestinal tract. Some cytokines such as IL-3 and IL-5 are responsible for the recruitment of eosinophils that subsequently infiltrate the digestive mucosa causing histological damage.
Clinical Presentation
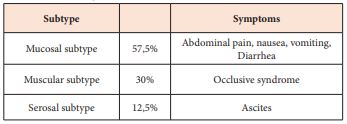
Symptoms of EGE are nonspecific and can be seen in various other gastrointestinal disorders. The clinical presentation depends on the location of the disease and the depth of the histological damage. The mucosal subtype is the most commonly reported one, patient may present with abdominal pain with nausea or vomiting. Severe symptoms may be observed: weight loss, malabsorption syndrome, exudative enteropathy and growth retardation in children [6,7]. The muscular subtype is characterized by infiltration of eosinophils in the muscle layer, causing symptoms of intestinal obstruction explained by bowel wall thickening. Patients present with abdominal ascites in the serosal form (Table 2). A history of allergy is often reported: food allergy, asthma, allergic rhinitis and eczema.
Table 2: Clinical signs.
Laboratory Findings
Blood hypereosinophilia is often present with higher levels in patient with serosal pattern but can sometimes be missing [8]. An absolute count >600 cells/mm3 indicates peripheral hpereosinophilia. The absence of eosinophilic disorde does not rule out the diagnosis [9]. Ig E levels can be elevated in children and support the diagnosis [4]. A parasitological examination of the stool (to be repeated over 3 days) should be carried out in order to eliminate a parasitic infection. HIV infection test should also be performed.
Endoscopy
Endoscopy is an important step in the diagnosis of EGE. Several endoscopic aspects have been reported. The mucosa may be normal or has nonspecific findings: mucosal erythema, ulcerated mucosa, sometimes mucosal nodules can also be seen [10]. Gastric ulcers have been reported in the literature. Endoscopy remains non-specific for the diagnosis of EGE. The unequal distribution of eosinophils requires several biopsies, at least five or six, to be performed from normal and pathological mucosa to avoid sampling errors [11].
Pathology
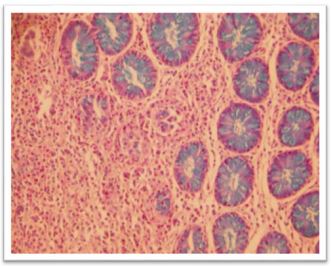
Histopathological examination confirms the diagnosis. Definition of EGE is based on eosinophils count exceeding more than 20 per HPF on microscopic examination (Figure 1). Eosinophilic disorder in the lamina propria of the mucosa is physiological and is sometimes associated to many pathological conditions. The presence of eosinophils in the submucosa, serosa is always pathological [12]. During EEG, histological damage is discontinuous, explaining the polymorphism of clinical signs. Obtaining multiple samples throughout the digestive tract, including normal areas is helpful in establishing the diagnosis of EGE.
Figure 1: Eosinophilic colitis: histological aspect (hemataxylin and eosin × 100).
Treatment
Treatment is based on the severity of the clinical manifestations. Some patients improve spontaneously while others have a persistent disease. In case of an identified food allergy, dietary elimination can improve the clinical symptoms. The exclusion regime can be tried for a period of six weeks (six-food elimination diet without soya, wheat, eggs, milk, peanuts, and crustaceans) [13]. However, it is possible that EEG may progress and affect other segments of the digestive tract. If eviction regimen has failed daily doses of prednisone ranging from 20 to 40 mg (1–2 mg/kg per day) for 2 to 6 weeks should be used. Methylprednisolone instead of prednisone may also be recommended [13]. An alternative to systemic steroids is budesonide (0.25mg twice daily to 9 mg daily in a single dose). Budesonide has been shown to be effective [14]. Prescribing proton pump inhibitors can be effective on symptoms even in the absence of gastroesophageal reflux [15]. Immunomodulators such as azathioprine and 6-mercaptopurine have good results and have been proposed by some authors to address the side effects of corticosteroids. The use of anti-tumor necrosis factor (TNF)-α in the treatment of severe adult EGE has been reported [16]. Other therapeutic classes have been described but are rarely used in current practice and are still considered experimental: ketotifen (mast-cell-membrane-stabilizing and antihistaminic effect), montelukast (competitive leukotriene receptor antagonist) [17].
Conclusion
EEG is a rare under-diagnosed disease. However, good communication between clinicians, endoscopists and pathologists can help to better diagnose this pathology. Prospective and randomized clinical trials to evaluate the best available treatments are still lacking. Therefore, it is essential to develop a health strategy for the effective management of EGE. Further studies are needed to compare the efficacy and safety profiles of the different treatments available and to select predictive factors of relapse.
References
- Rothenberg ME (2004) Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol 113(1): 11-28.
- Jensen ET, Martin CF, Kappelman MD, Dellon ES (2016) Prevalence of eosinophilic gastritis, gastroenteritis, and colitis: estimates from a national administrative database. J Pediatr Gastroenterol Nutr 62(1): 36-42.
- Chen MJ, Chu CH, Lin SC, Shih SC, Wang TE (2003) Eosinophilic gastroenteritis: clinical experience with 15 patients. World J Gastroenterol 9(12): 2813-2816.
- Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR (1990) Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut 31(1): 54-58.
- Lehman HK, Lam W (2019) Eosinophilic Esophagitis. Pediatr Clin North Am 66(5): 955-965.
- Reed C, Woosley JT, Dellon ES (2015) Clinical characteristics, treatment outcomes, and resource utilization in children and adults with eosinophilic gastroenteritis. Dig Liver Dis 47(3): 197-201.
- Ridolo E, Melli V, De Angelis G, Martignago I (2016) Eosinophilic disorders of the gastro-intestinal tract: an update. Clin Mol Allergy 14-17.
- Uppal V, Kreiger P, Kutsch E (2016) Eosinophilic Gastroenteritis and Colitis: a Comprehensive Review. Clin Rev Allergy Immunol 50(2): 175-188.
- Zhang M, Li Y (2017) Eosinophilic gastroenteritis: A state-of-the-art review. J Gastroenterol Hepatol 32(1): 64-72.
- Sunkara T, Rawla P, Yarlagadda KS, Gaduputi V (2019) Eosinophilic gastroenteritis: diagnosis and clinical perspectives. Clin Exp Gastroenterol 12(1): 239-253.
- Katsumi N, Yamaguchi Y, Yamato T, Morozumi K, Abe T, et al. (2002) Multiple ulcerative lesions of the stomach: A rare case of eosinophilic gastroenteritis. Gastrointest Endosc 56(5): 762-764.
- Blackshaw AJ, Levison DA (1986) Eosinophilic infiltrates of the gastrointestinal tract. J Clin Pathol 39(1): 1-7.
- Gupta N, Aggarwal A, Gupta R, Sule S, Wolf DC (2015) The management of eosinophilic gastroenteritis. Scand J Gastroenterol 50(11): 1309-1314.
- Lombardi C, Salmi A, Passalacqua G (2011) An adult case of eosinophilic pyloric stenosis maintained on remission with oral budesonide. Eur Ann Allergy Clin Immunol 43(1): 29-30.
- Yamada Y, Toki F, Yamamoto H, Nishi A, Kato M (2015) Proton pump inhibitor treatment decreased duodenal and esophageal eosinophilia in a case of eosinophilic gastroenteritis. Allergol Int 64: S83-S85.
- Turner D, Wolters VM, Russell RK, Shakhnovich V, et al. (2013) Anti-TNF, infliximab, and adalimumab can be effective in eosinophilic bowel disease. J pediatr gastroenterol Nutr 56(5): 492-497.
- De Maeyer N, Kochuyt AM, Van Moerkercke W, Hiele M (2011) Montelukast as a treatment modality for eosinophilic gastroenteritis. Acta Gastro-Ent Belg 74(4): 570-575.