Is There any Association between Blood Group and Impacted Third Molars?
Farhad Ghorban*
Shahid Rajaee Teacher Training University, Iran
*Corresponding author: Farhad Ghorban, Shahid Rajaee Teacher Training University, Lavizan Area,16785-163, Iran
Article History
Received: March 25, 2021 Accepted: May 04, 2021 Published: May 07, 2021
Citation: Ghorban F. Is There any Association between Blood Group and Impacted Third Molars? Int. J. Orl. Health. 2021;1(2):25‒28. DOI: 10.51626/ijoh.2021.01.00006
Abstract
Background: Blood type is an important genetic characteristic that is inherited from parents’ thorough alleles, and might be related to several problems, including, dental conditions. In the present study we examined the probable association of impacted teeth and blood groups.1.2
Methods: This retrospective study was done on patients who were referred for obtaining oral radiographs. For each blood group and Rh factor, we randomly selected 40 patients. The type of blood group of the participants was also obtained from the medical records available in the patients’ history archives.
Results: A total of 320 participants contributed to the study, 136(42%) were males and 184(57%) were females. The mean age was 29 ± 6 years. Among all participants, 205(64%) had no impacted third molar, 26(8%) had one impacted third molar, 43(13%) had 2 impacted third molars, 5(1%) had 3 impacted third molars, and 41(12%) had 4 impacted molars.
Conclusion: In the present study no significant association was found between ABO blood groups and impacted third molars.
Keywords: Blood group; Impacted Molar; Rh Factor
Background
Impaction is diagnosed when one or more teeth cannot fully erupt to the correct position in the oral cavity [1-4]. The prevalence of the condition seems to be higher in the maxilla and female gender [5,6]. The third molars are considered to be the most susceptible sites for the impaction, following by second mandibular premolar and second mandibular molar [1,4]. The factors that increase the risk of impaction are mostly related to the conditions that are because of genetical problems, such as, cleidocranial dysplasia, primary failure of eruption, local and environmental reasons such as premature loss and retained deciduous teeth, malposed and ankylosed teeth, the discrepancy between the jaws, lack of space or tooth crowding, the wrong path of eruption, rotation of tooth buds, some barrier like other teeth special pathologic condition such as cyst or odontoma [1,3-5,7,8]. Untreated impacted teeth may cause some problems such as periodontal and pulp diseases, temporomandibular joint disorders, damage to the distal surface of adjacent teeth, crowding, and oral and maxillofacial cysts and tumors [9-11]. The treatment of impacted tooth is consisted of conservative follow-up, orthodontic interventions, repositioning of the teeth, and extraction of the teeth in the in the cases of oral pain, infection, resorption, or cyst [6,12].
Blood type is inherited from parents through the alleles and might be related to some problems and diseases [13]. The most common categorization of the blood types is ABO classification, as the blood groups are classified into four subtitles depending on the presence and absence of A and B antigens on the hemoglobin, and anti-A and anti-B antibodies in the human body [14]. Blood type O expresses neither A nor B antigen, blood type AB contains both A and B antigens, blood type A has an A antigen on the red cells, and blood group B has B antigen on the red cells [13]. The next common blood group system is the Rhesus (Rh) system that is based on the R protein found on the surface of the blood cells [15]. Rh-positive and Rh-negative present Rh antigen on the red blood cell or not, respectively [16]. Several studies have mentioned that the types of blood groups and oral problems, including, periodontal diseases, and caries could be related (14). For example, it has been shown that the prevalence of dental caries is lower in individuals with blood group A, and children with blood group AB are more susceptible to early childhood caries [14,17].
However, there is still controversial results regarding the relationship between ABO blood groups and the incidence of oral and dental diseases. The controversial pieces of evidence on this matter could be due to the various geographical and genetical contributions of blood groups in different populations [18]. While finding new comprehensive methods to predict dental problems is an important task that could reduce the future complications, few investigations have statistically determined the association of blood group and oral problems. The present study aimed to evaluate the association between ABO and Rh blood groups and the most common impacted tooth, bony impacted third molars.
Methods
Population
This is a cross-sectional study that was approved by the Department of Oral and Maxillofacial Surgery, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran. The study protocol was approved by the Medical Ethics Committee of Shiraz University of Medical Sciences by the Institutional Review Board (IRB) number of IR.SUMS.DENTAl.REC.1399.080.
All patients who referred to the Department of Oral Radiology to obtain panoramic images for an oral examination or dental procedures from March 2019 to May 2020 were included in the study. Since the frequency of blood group contribution was different in the population, to reduce the bias, we selected an equal number of subjects for each blood group type (40 subjects were selected for each blood group and Rh factor), and a total of 320 subjects were enrolled in this study.
The study was completely explained to each participant and a signed informed consent was obtained. Inclusion criteria were patients aged more than 24 years who had high quality panoramic radiographs, and those who were willing to take part in the study. Exclusion criteria were patients with systemic problems or congenital syndromes, craniofacial deformities, jaw pathology lesions and previous trauma, lack of information about their blood groups, primary teeth dentition, and history of dental extraction. All individuals were assigned by a single operator and radiographic device.
Study design
All individuals were interviewed by a single practitioner (author). Clinical oral examination and x-ray panoramic investigation were done to determine the presence or absence of bony impacted teeth. A separate sheet containing information on sex, age, blood group type, and the number of impacted teeth (if there are) was used as a record for each individual. Blood groups of patients were obtained from medical records, patients’ blood and organ donation cards, and driving licenses. If the participants had impacted tooth, the number and the site of the teeth were written on the sheet.
Statistical analysis
Descriptive statistics including mean, standard deviation, and frequency were computed. Chi-square test was used to determine the relationship between ABO blood groups and the prevalence of impacted teeth. P values < 0.05 were considered as significant. All the statistical tests were performed using Statistical Package for the Social Sciences (SPSS version, 23). Microsoft Word and Excel were used to generate graphs and tables.
Results
A total of 320 participants contributed to the study; 136(42%) subjects were males and 184(57%) were females. Their mean age was 29 ± 6 years. Among them, 205 participants (64%) had no impacted third molar, 26(8%) had one impacted third molar, 43(13%) had 2 impacted third molars, 5 (1%) had 3 impacted third molars, and 41(12%) had 4 impacted molars. It was seen that 111(34%) of the females and 94(29%%) of the males had no impacted third molar. Shows that more females presented impacted third molar, but there was no significant association between gender and impacted third molar (P >0.005).
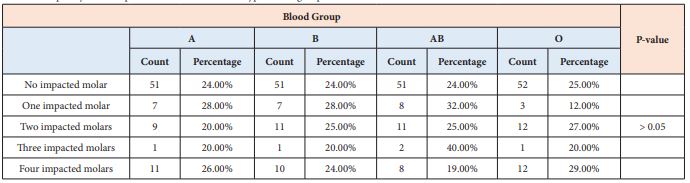
Our data showed that the subjects with no impacted third molar in the blood groups A, B, AB, and O were distributed as 51(24%), 51(24%), 51(24%), and 52(25%); additionally, the prevalence of subjects with four impacted third molar in the blood groups A, B, AB, and O was distributed as 11(26%), 10(24%), 8(19%), and 12(29%) (Table1).
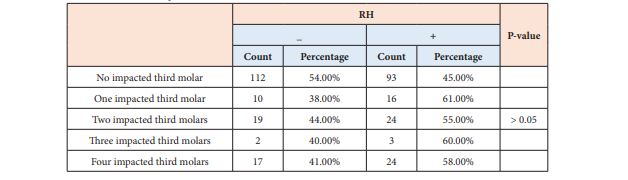
Among participants with no impacted third molar, 112(54%) of them were RH negative and 93(45%) were RH positive. Table 2 shows the association between the RH factor and impacted teeth. Moreover, among the participants with four impacted third molars, 17(41%) were RH negative and 24(58%) were RH positive.
Table 1: Frequency of the impacted third molar in blood types blood group.
Table 2: Association between RH factor and impacted teeth.
Chi-square test showed the association of blood groups and RH factor with impacted third molar was statistically non-significant (P >0.05), which means there was no association between blood group and RH factor with a prevalence of impacted third molar.
Discussion
Third molars are the most common impacted teeth in the oral cavity [7]. General dentists or specialists find impacted teeth throughout routine dental check-ups by taking periapical, occlusal, or panoramic radiographic images [2,19]. The most common technique to diagnose the impacted teeth is orthopantomography (OPG) due to fastness, low cost, low radiations dosage, and illustration of bilateral view of the mandible [7]. Some dentists prefer to use three-dimensional information like cone beam computed tomography (CBCT) or low dose computed tomography (CT) due to some restrictions of two-dimensional radiographs, such as the inability to measure the buccolingual dimensions [19,20].
The most common reason for impacted molar is inadequate space of the jaws [20]. Furthermore, the jaw growth was controlled by genes, as previous study showed that genetic factors guide the jaw space [21]. Furthermore, it is reported that jaw dimensions are strongly affected by the genetic component [22]. According to the previous evidence we hypothesized that inherent factors involving in characterization of blood groups would play a role in the impaction of the third molar. Hence, we might be able to use blood group type as an indicator of third molar impaction.
Blood types are important regarding blood transfusion, but some studies have shown the relationship between different blood groups and some diseases; for example, individuals with blood groups A and B are more prone to atherosclerosis, or a correlation between developmental cholelithiasis, gastric ulcer, and gastric carcinoma was found in the people with blood group A [23-25]. Also, Kaur et al. [26] revealed that individuals with blood group O had a higher risk of hypertension. Another study demonstrated that individuals with blood groups O and A were more likely to catch H. Pylori infection [27]. Other studies revealed the relationship between blood types and congenital cataract in the Asian race [28,29]. Furthermore, individuals with blood group A have a greater risk and people with blood group O are at the lower risk of getting coronavirus disease-19 [30].
Moreover, some studies revealed that there is a relationship between blood groups and increased incidence of oral diseases such as periodontitis. The first research that showed such relationship was done in 1930, and found an association between blood groups and periodontal diseases [31,32]. Besides, people with blood group A are more prone to gingivitis, or periodontitis is more prevalent in individuals with blood group O [18]. People with blood group B are at a higher risk of aggressive periodontitis, and individuals with blood group A are at higher risks of severe alveolar bone loss [33]. It was found that advanced forms of generalized periodontitis were more common in people with blood types O and A in comparison with blood groups B and AB [34]. Studies have mentioned that people with blood groups A and B have more malocclusion, and those with blood group B have a greater rates of maxillofacial deformities [35,36]. Besides, Nikawa et al. [37] reported that among denture wearers individuals with blood group O were more prone to denture stomatitis [37].
Conversely to the above-mentioned evidence, no association was found between the non-secretor status of ABO blood group antigens and localized juvenile periodontitis [38]. Some studies evaluated the relationship between the blood group and malocclusion, they found that blood groups have no association with malocclusions [39,40]. Our data also showed that there was a higher percentage of blood group O in patients with impacted third molars; however, no significant association was shown.
The results of our study might have been affected by some limitations. One of the most important weaknesses of our study is that all of our participants were Iranian, while different ethnicities should be investigated to estimate the relationship between blood group and impacted teeth. A rising number of participants of both genders, different ages, and blood types are needed to be investigated in this regard.
Conclusion
The evaluation of the relationship between blood group and impacted third molar revealed that blood groups have no association with the impacted third molar. However, more studies with higher and diversified participants should be done in order to find comprehensive results.
References
- Fardi A, Kondylidou-Sidira A, Bachour Z, Parisis N, Tsirlis A, et al. (2011) Incidence of impacted and supernumerary teeth-a radiographic study in a North Greek population. Med Oral Patol Oral Cir Bucal 16(1): e56-e61.
- Hamada Y, Timothius CJC, Shin D, John V (2019) Canine impaction–A review of the prevalence, etiology, diagnosis and treatment. Seminars in Orthodontics. 25(2): 117-123.
- Kramer RM, Williams AC (1970) The incidence of impacted teeth: a survey at Harlem Hospital. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 29(2): 237-241.
- Al-Zoubi H, Alharbi AA, Ferguson DJ, Zafar MS, Muhammad Sohail Zafar (2017) Frequency of impacted teeth and categorization of impacted canines: A retrospective radiographic study using orthopantomograms. Eur J Dent 11(1): 117-121.
- Nowzari H, Rodriguez AE (2019) Impacted teeth: Closed flap surgery. J Esthet Restor Dent 31(3): 233-239.
- Dachi SF, Howell FV (1961) A survey of 3,874 routine full-mouth radiographs: II. A study of impacted teeth. Oral Surg Oral Med Oral Pathol 14(10): 1165-1169.
- Al-Gunaid TH, Bukhari AK, El Khateeb SM, Yamaki M (2019) Relationship of mandibular ramus dimensions to lower third molar impaction. Eur J Dent 13(02): 213-221.
- Suri L, Gagari E, Vastardis H (2004) Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature review. Am J Orthod Dentofacial Orthop 126(4): 432-445.
- Hou R, Kong L, Ao J, Liu G, Zhou H, et al. (2010) Investigation of impacted permanent teeth except the third molar in Chinese patients through an X-ray study. J Oral Maxillofac Surg 68(4): 762-767.
- Li D, Tao Y, Cui M, Zhang W, Zhang X, Hu X, et al. (2019) External root resorption in maxillary and mandibular second molars associated with impacted third molars: a cone-beam computed tomographic study. Clin Oral Investig 23(12): 4195-4203.
- Mortazavi H, Baharvand M (2016) Jaw lesions associated with impacted tooth: A radiographic diagnostic guide. Imaging Sci Dent 46(3): 147-157.
- Frank CA (2000) Treatment options for impacted teeth. J Am Dent Assoc 131(5): 623-32.
- Watkins W (2001) The ABO blood group system: historical background. Transfus med 11(4): 243-265.
- Yadav K, Solanki J, Dileep CL, Adyanthaya BR, Mishra P, et al. (2018) Association between different blood groups, depression and oral health status of dental students. Clujul Med (1957) 91(3): 317-21.
- Avent ND, Reid ME (2000) The Rh blood group system: a review. Blood 95(2): 375-387.
- Abbas A, Abbas B, Aziz S, Ullah F, Panhwar WA, Ali A, et al. (2020) Prevalence of ABO and Rh Blood Group in District Karak (Female). Bull Env Pharmacol Life Sci 29(2): 31-34.
- Govindaraju L, Jeevanandan G, Subramanian E (2018) ABO blood grouping: A potential risk factor for early childhood caries-A cross-sectional study. Indian J Dent Res 29(3): 313-316.
- Koregol AC, Raghavendra M, Nainegali S, Kalburgi N, Varma S, et al (2010) ABO blood groups and Rhesus factor: An exploring link to periodontal diseases. Indian J Dent Res 21(3): 364-368.
- Guerrero M, Shahbazian M, Elsiena Bekkering G, Nackaerts O, Jacobs R, et al. (2011) The diagnostic efficacy of cone beam CT for impacted teeth and associated features: a systematic review. J Oral Rehabil 38(3): 208-216.
- Kaczor-Urbanowicz K, Zadurska M, Czochrowska E (2016) Impacted Teeth: An Interdisciplinary Perspective. Adv Clin Exp Med 25(3): 575-585.
- Trakiniene G, Sidlauskas A, Trakinis T, Andriuskeviciute I, Salomskiene L, et al. (2018) The Impact of Genetics and Environmental Factors on the Position of the Upper Third Molars. J Oral Maxillofac Surg 76(11): 2271-2279.
- Savoye I, Loos R, Carels C, Derom C, Vlietinck R (1998) A genetic study of anteroposterior and vertical facial proportions using model-fitting. Angle Orthod 68(5): 467-470.
- Stakishaitis D, Ivashkiavichene L, Narvilene A (1991) Atherosclerosis of the coronary arteries and the blood group in the population of Lithuania. Vrach Delo 8: 55-57.
- Jesch U, Endler PC, Wulkersdorfer B, Spranger H (2007) ABO blood group. Related investigations and their association with defined pathologies. Scientific World Journal 7: 1151-1154.
- Chukwurah E, Mbah A (2004) Relationship between human ABO blood groups and enteric fever. Journal of Health and Visual Sciences 6(3).
- Kaur M (2017) Association between ABO Blood Group and Hypertension among Post-menopausal Females of North India. The Anthropologist 17(2): 677-680.
- Kanbay M, Gur G, Arslan H, Yilmaz U, Boyacioglu S, et al. (2015) The relationship of ABO blood group, age, gender, smoking, and Helicobacter pylori infection. Dig Dis Sci 50(7): 1214-1217.
- Reid ME, Bird GW (1994) Associations between human red cell blood group antigens and disease. Transfus Med Rev 4(1): 47-55.
- Issitt PD (1993) Null red blood cell phenotypes: associated biological changes. Transfus Med Rev 7(3): 139-155.
- Zhao J, Yang Y, Huang HP, Li D, Gu DF, et al. (2020) Relationship between the ABO Blood Group and the COVID-19 Susceptibility.
- Ishikawa I (2007) Host responses in periodontal diseases: a preview. Periodontology 2000 43(1): 9-13.
- Mahajan N, Kohad R (1998) Association between ABO blood groups and periodontal diseases. JISP 1(02): 62-3.
- Kaslick RS, Chasens AI, Tuckman MA, Kaufman B (1971) Investigation of periodontosis with periodontitis: Literature survey and findings based on ABO blood groups. Periodontol 42(7): 420-427.
- Bandrivsky YL, Bandrivska OO, Shkrebnyuk RY, Dyryk VT (2020) Prevalence of the generalized periodontitis in patients with different groups blood in depending on age and periodontal biotype. Wiad Lek 73(1): 119-122
- Gheisari R, Ghoreishian M, Bijan M, Amrolah R, et al. (2008) The association between blood groups and maxillofacial deformities. Indian J Plast Surg 41(02): 138-140.
- Haque S, Ab Rahman WSW (2018) Agenesis of Third Molar Tooth Germs in Relationship with ABO Blood Group in Orthodontic Patients. International Medical Journal 25(4): 2592-2662.
- Nikawa H, Kotani H, Sadamori S, Hamada TJT (1991) Denture stomatitis and ABO blood types 66(3): 391-394.
- Frias MT, Lopez NJ (1994) No association between secretor status of ABO blood group antigens and juvenile periodontitis. Acta Odontol Latinoam 8(2): 9-15.
- Gupta SPJEDs (2018) Association of ABO blood groups with occlusal pattern among Orthodontic patients of Kathmandu district. EC Dental Science 17(12): 2119-2219.
- Shokor F, Rahman W, Alam MK (2015) Craniofacial morphology with genetic influence of ABO blood Group in Malaysian orthodontic patients. IJPBS 6(4): 412-418.